-
PDF
- Split View
-
Views
-
Cite
Cite
S Rymaruk, CE Owers, R Ackroyd, Aortic thrombus after bariatric surgery, Journal of Surgical Case Reports, Volume 2012, Issue 5, May 2012, Page 1, https://doi.org/10.1093/jscr/2012.5.1
Close - Share Icon Share
Abstract
Laparoscopic gastric bypass is becoming a frequently performed bariatric operation for patients with obesity. However, bariatric surgery has inherent risks and complications, which are further potentiated by the high risk nature of bariatric patients. These complications can be either site specific i.e. anastomotic leaks, or systemic i.e. venous thromboembolism, however they can intimately related. We present the case of one patient undergoing routine gastric bypass complicated postoperatively by recurrent intra-abdominal collections and sepsis, and aortic thrombosis with distal embolisation.
INTRODUCTION
Laparoscopic gastric bypass surgery is amongst the most frequently performed operations in bariatric surgery. We report the case of one patient undergoing routine gastric bypass who experienced major complications.
CASE REPORT
A 56 year old female was referred from a district general hospital after a protracted history of abdominal pain and vomiting. Past medical history included osteoarthritis and hypertension, and a past surgical history of laparoscopic Roux-en-Y gastric bypass in 2008 (pre-operative BMI of 48 Kg/m2).
A contrast swallow on admission showed evidence of multiple small bowel strictures. A laparotomy and revision of Roux-en-Y gastric bypass was undertaken with post operative management on HDU, but the patient had ongoing problems with pain and wound discharge. A CT scan revealed a 7cm collection adjacent to the alimentary limb which was percutaneously drained under ultrasound guidance.
Due to clinical deterioration, a further CT was performed which demonstrated a large communicating collection filling the paracolic gutters and pelvis, with a multiloculated left lobe liver abscess, and a smaller abscess in the right lobe (figure 1). This was percutaneously drained and there was clinical improvement. The patient was discharged home.
The patient re-presented 2 weeks later with increasing epigastric pain and malaise. Imaging showed a persistent collection in the pelvis and liver, and a further two percutaneous procedures were performed.
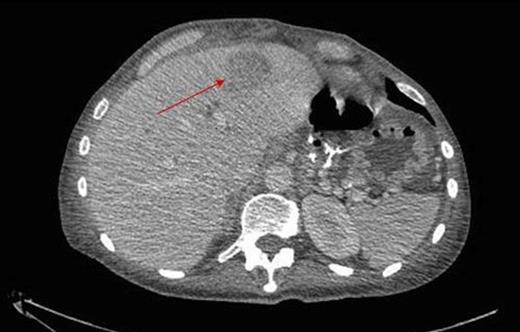
During inpatient stay, she became haemodynamically unstable with spiking temperatures and an elevating white cell count. She also complained of bilateral discolouration of her toes and examination revealed increasing oedema with diminished pedal pulses. A contrast CT scan of the abdomen confirmed ongoing collections with evidence of an aortic thrombus extending into the left iliac artery, presumed to be the embolic source for her vascular findings (figure 2 & 3). She underwent a further laparotomy and washout, and was heparinised postoperatively. There was resolution of vascular symptoms and evidence of improvement in peripheral perfusion postoperatively, and the patient was eventually discharged.

Thrombus within the distal aorta shown by a filling defect (red arrow)

Extension into the left iliac artery shown by a filling defect (red arrow)
DISCUSSION
Surgery has inherent risks and complications, which may be further be potentiated by the high risk nature of bariatric patients. A systematic review of the literature concluded that peri-operative complications were encountered more frequently in bypass patients compared to those undergoing laparoscopic gastric banding (9% and 5%), although long-term re-operation rates were lower (16% and 24% respectively) (1). The mortality of both bypass and band operations were low (0.17% and 0.06%). Further systematic reviews have reported major early complications rates of gastric bypass surgery as 6.3%, with major complications including death (0.2%), perforation (0.5%), venous thromboembolism (0.3%), significant postoperative bleed (0.9%), postoperative infection (2.9%) and anastomotic leaks (0.9%) (1).
Despite these risks gastric bypass is an effective operation for obesity; one study reported 76% excess body weight loss and a 78% resolution of diabetes at 1 year in patients undergoing bypass compared to 48% weight loss and 50% diabetes resolution in patients undergoing banding (2). Generally high levels of patient satisfaction are recorded, estimated to approach 80% (3).
Venous thrombosis is well documented in the literature as a complication of obesity and bariatric surgery. One study reported an incidence of deep vein thrombosis in the group of 500 consecutive patients to be 0.2% (4). However, there is little data regarding arterial thrombosis as a complication of bariatric surgery.
There are numerous predisposing factors to arterial thrombosis within this clinical picture. Bariatric patients have significant risk factors for atherosclerotic disease, both due to obesity, and to secondary diseases such as hypertension and diabetes, which may develop as part of the metabolic syndrome. However, with this patient there was no evidence of aortic thrombosis on previous imaging, and a new presentation of clinical signs and symptoms would be in keeping with a new onset thrombosis.
There are also factors relating to a hypercoagulable state, which in this patient could be numerous. This patient had recurrent episodes of sepsis, which is well known to precipitate hypercoagulability, which at the severe end of the spectrum, exists disseminated intravascular coagulation (DIC). Sepsis mediated hypercoagulability occurs as a result of the activation of inflammatory and coagulation cascades (5). Dehydration secondary to both poor intake and insensible losses through either infection or surgery may also cause an increased coagulable state. Inflammatory and hypercoagulation may be due to the direct effects of surgery through the stress response (6).
Roux-en-Y gastric bypass is deemed a safe operation in the management of obesity. It generally has low complications and high patient satisfaction (1-3). We present a case complicated postoperatively by recurrent intra-abdominal collections and sepsis, and aortic thrombosis with distal embolisation.



