-
PDF
- Split View
-
Views
-
Cite
Cite
S Rymaruk, A Razak, R McGivney, Metallosis, psoas abscess and infected hip prosthesis in a patient with bilateral metal on metal total hip replacement, Journal of Surgical Case Reports, Volume 2012, Issue 5, May 2012, Page 11, https://doi.org/10.1093/jscr/2012.5.11
Close - Share Icon Share
Abstract
Metal on metal hip (MoM) resurfacing / replacement has recently been one of the most discussed topics in orthopaedics. Significant revision rates and complications are associated with MoM. We report a patient presenting with infection of a total hip prosthesis in conjunction with a psoas abscess in which the presentation is complicated by radiological evidence of suspected metallic debris in the lower limb tissues and elevated chromium and cobalt levels, suggestive of metallosis secondary to MoM.
INTRODUCTION
Metal on metal hip (MoM) resurfacing / replacement has recently been one of the most discussed topics in orthopaedics. Revision rates are high according to the British NJR database (1). Complications related to MoM include metallosis, pseudotumour and ALVAL (2).
We present a case of psoas abscess and infected hip prosthesis in a patient with suspected metallosis secondary to metal on metal total hip replacement. To our knowledge there has been no such cases in the literature.
CASE REPORT
A 49 year old male patient presented to the medical admissions unit with a one week history of left hip and thigh painful swelling. The only past medical history was bilateral metal on metal total hip replacements four years prior, the indication osteoarthritis (figure 1). The patient had no problems regarding the hips since surgery.

AP Pelvis radiograph demonstrating bilateral metal on metal total hip replacements
The patient was found to have gross swelling of the entire left leg, with overlying erythema. Observations revealed a low grade pyrexia. Blood investigations showed a neutrophilic leukocytosis with deranged renal and liver function, and prolonged INR. Blood analysis had been normal the year before. The clinical impression at time of admission was DVT or sepsis. The key differential diagnoses included deep vein thrombosis, cellulitis, necrotising fasciitis, septic arthritis, metallosis, and psoas abscess.
The patient underwent a Doppler scan which ruled out a DVT, then a CT scan of the left hip and thigh (figure 2). This demonstrated generalised superficial oedema with a small collection over the lateral thigh, and an irregular low density appearance of the gluteus and psoas muscles. With progressive deterioration in clinical state, the patient underwent ultrasound scanning of the thigh and hip. This demonstrated a small hip effusion with a large gas containing echogenic collection in the left psoas muscle (figure 3).

Axial CT demonstrating an irregular low density appearance within the left psoas (red arrow) and gluteal muscles (blue arrow)
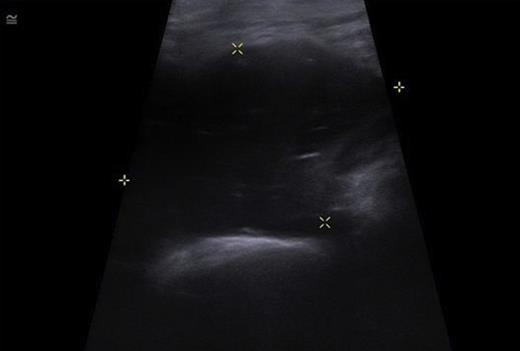
USS of the hip demonstrating a large echogenic collection in the left psoas containing gas.
The patient underwent ultrasound guided drainage of 300ml of pus. Due to ongoing clinical concerns regarding the possibility of metallosis, the patient underwent blood sampling for cobalt and chromium levels, and was imaged with MRI. Chromium and cobalt levels returned elevated (117nmol/L and 169nmol/L), and MRI demonstrated the resolving psoas collection but low signal foci around the left hip which could represent metallic debris (figure 4).
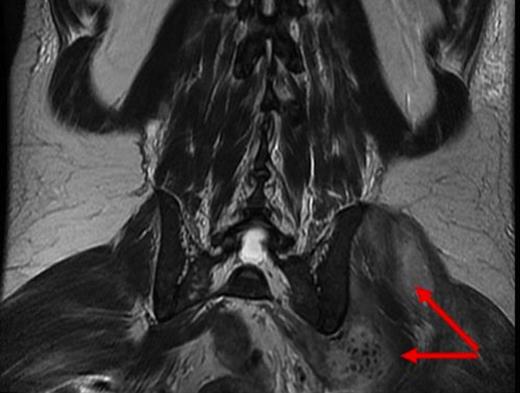
coronal MRI demonstrating ongoing collections around the left hip with low signal foci which may represent metallic debris (red arrow)
The patient underwent exploration and drainage of the thigh collection which demonstrated an infective tract coming from the hip joint. After a 3 week course of intravenous antibiotics, the patient improved clinically. The patient was discharged home, but has been referred for revision arthroplasty surgery of the hip at which time histological analysis will take place to aid a formal diagnosis of metallosis.
DISCUSSION
There are several factors that were contributing to this patients hip pain; psoas abscess formation, infected total hip prosthesis, and suspected metallosis.
The true incidence of psoas abscess is unknown, but thought to be under reported (3,4). The relationship between psoas abscess and joint infection is understood, but it is difficult to ascertain which is the initiating event. Reports of psoas abscess associated with prosthetic hip infections has only rarely been reported in the literature, but a study concluded that 12% of patients with hip prostheses infections were complicated by psoas abscess formation (5). They hypothesised that the association was due to either direct spread through the bursa, or acetabular fissures arising at the time of surgery which allowed the initial infection to extend. Two case reports have also been published in the literature reporting the spread of infection to be the reverse direction of this, from an initial psoas abscess to a hip prosthesis (6,7).
The findings of elevated cobalt and chromium on a background of MRI suggestive metallic debris, further complicates the clinical picture. Metallosis secondary to metal on metal arthroplasties have been reported in the literature. A study described 4 patients presenting with groin pain after metal-on-metal hip resurfacing, with histological analysis in keeping with an immunologic response due to metal sensitivity (8). Another study postulated that there was an increased risk of infection in patients with metallosis since the combination of metal debris, ALVAL and tissue necrosis provided an optimum environment for peri-prosthetic bacterial growth and rapid spread of infection (9). A case report described a patient with an infected hemiarthroplasty which was associated with a retroperitoneal abscess in the presence of metallosis which was diagnosed by low signal areas on MRI scanning (10).
In summary, this complex case reports the occurrence of a prosthetic hip joint infection in association with a psoas abscess formation, on a background of suspected metallosis.



