-
PDF
- Split View
-
Views
-
Cite
Cite
SP Carmichael, LD Procter, AC Bernard, A novel treatment for inferior mediastinal abscess via abdominal laparoscopy, Journal of Surgical Case Reports, Volume 2012, Issue 4, April 2012, Page 7, https://doi.org/10.1093/jscr/2012.4.7
Close - Share Icon Share
Abstract
Mediastinal abscess can be managed through a variety of both invasive and minimally invasive methods, as determined by location and spread of infection. Thoracotomy remains the gold standard in treatment and is often employed. In the present case, a 54-year-old female with chronic pancreatitis presented with a 1-week history of severe epigastric pain, nausea and vomiting. On CT scan, a large abscess was discovered in the anterior inferior mediastinum. She was taken to the operating room and underwent laparoscopic drainage of the abscess. Laparoscopy represents a novel approach in management of anterior inferior mediastinal abscess.
INTRODUCTION
Mediastinal abscess is a rare yet emergent infection of the thoracic cavity connective tissue, resulting from multiple potential sources: esophageal perforation (Boerhaave’s syndrome), odontogenic and peritonsillar abscess (descending necrotizing mediastinitis), cardiovascular or thoracic surgical procedures, trauma or rarely due to hematogenous spread (1,2). Clinical diagnostic signs include dysphagia, dyspnea, fever, and chest pain with the potential for septic shock, as the disease progresses (3). Water-soluble barium contrast swallow, transcutaneous ultrasound, chest radiograph, and CT are frequently utilized tools for visualization and prognosis (3,4).
The foremost aim in management of mediastinal abscess is early debridement and drainage (5). While thoracotomy remains the gold standard of treatment, this approach carries significant risk of complication in certain populations (3,5). Minimally invasive options such as, video-assisted thoracoscopic surgery (VATS), CT guided percutaneous drainage, cervical drainage (irrigation/suction) and trans-esophageal endoscopic ultrasound (EUS) represent safe and effective management strategies, in certain cases (4-6). Herein is reported a novel application of laparoscopy as an additional alternative approach to drainage of anterior inferior mediastinal abscess.
CASE REPORT
A 54-year-old female with a history significant for alcohol abuse, surgical correction of annular pancreas 20 years ago and chronic pancreatitis presented to a rural emergency department with a 1-week history of worsening severe epigastric pain, nausea and vomiting. She was in baseline health until 2 months prior when she first noticed episodic epigastric pain that was stabbing in nature. The patient was transferred to our institution for surgical evaluation based on an external department CT raising concern of possible diaphragmatic herniation versus fluid collection. Re-scan of the abdomen confirmed a fluid collection of 8-10 cm in the extra-peritoneal space of the intra-abdominal wall, extending superiorly to the anterior mediastinum. Subsequent laparoscopy revealed dense omental adhesions encapsulating an abscess cavity, which tracked into the inferior mediastinum. Purulent material was evacuated, fluid was sampled for bacterial culture and a Blake drain was placed. There was no evidence of existing mesh, intestinal fistula or enterotomy. The precise etiology of the abscess remains unclear. The patient was afebrile without leukocytosis throughout the hospital course and was discharged with clinic follow-up after 3 days of post-operative evaluation. At the one-month post-operative clinic visit, symptoms had resolved.
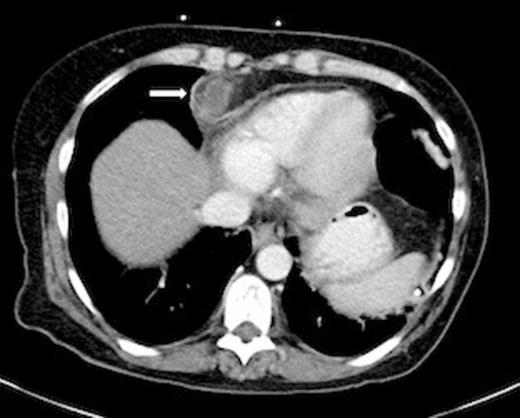
Axial CT Chest showing anterior inferior mediastinal abscess (Arrow).
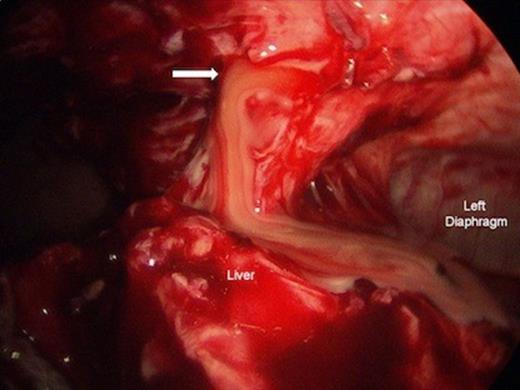
Laparoscopic drainage of anterior inferior mediastinal abscess. Left diaphragm and liver are shown. Arrow = Mediastinotomy.
DISCUSSION
Development of mediastinal abscess is inclusive of multiple etiologies (1,2). Given the location and encapsulation of the abscess in the presented case, descending mediastinitis from an oropharyngeal source seems unlikely. Similarly, the patient remained afebrile without leukocytosis throughout the hospital course thereby precluding hematogenous spread. There was no prior history of trauma or precipitating illness, by patient history. Most recent procedural history includes an unremarkable esophagogastroduodenoscopy and MRCP 2 years prior to presentation. Abscess fluid cultures from drainage revealed Prevotella intermedia, Haemophilus parainfluenzae and Streptococcus spp. At the time of procedure, the patient was not known to be immunosuppressed or receiving long-term corticosteroids. Taken together, these findings do not provide a definitive etiology for abscess development, though a role for recent instrumentation in the context of chronic inflammation and extensive abdominal surgical history may be suspected.
The management of mediastinal abscess is three-fold: early diagnosis, surgical drainage and appropriate antibiotic therapy (5). Location and extent of abscess and are both important factors in this determination. Transcervical drainage has been recommended by prior studies for management of mediastinal abscess at or above the level of the carina whereas thoracotomy or sub-xipoid incision is recommended for extensive sub-carinal abscesses (6). Recently, several investigators have shown video-assisted thoracoscopic surgery to be a successful alternative to open methods in mediastinitis management from multiple etiologies (3). Moreover, the effectiveness of non-invasive techniques has been demonstrated in cases of sub-carinal abscess (7). Such therapies may be preferable to more aggressive methods due to reduced risk of complication, less pain and more rapid recovery (5).
Successful employment of minimally invasive technique has also been shown recently in the management of Boerhaave’s syndrome (8,9). In this context, laparoscopy is utilized for primary repair of esophageal tear, gastrostomy, feeding jejunostomy, esophagomyotomy and harvesting of omentum (8). While local debridement of the posterior mediastinum is possible utilizing laparoscopic approach, thoracoscopy and VATS are often additionally utilized due to delays in diagnosis, extensive pleural contamination and post-procedural complication (9).
Percutaneous drainage is an alternative to surgical management of mediastinal abscess in subacute or well-defined fluid collections (10). Moreover, it represents the preferred course of treatment for intra-abdominal abscess and is a viable alternative to open drainage (10). Despite these factors, laparoscopy was undertaken in the present case due to the need for adequate inspection of the abdomen to exclude sources of pathology causal to abscess.
The treatment for mediastinal abscess remains controversial. While invasive technique may still represent the gold standard of therapy (6), we report the successful treatment of anterior inferior mediastinal abscess by laparoscopy in a 54 year-old female, without further complication. This method represents a novel approach to the management of abscess in this location without subsequent need for thoracoscopy or thoracotomy.



