-
PDF
- Split View
-
Views
-
Cite
Cite
V Vieira, H Alexandrino, E Furtado, F Martinho, Peritoneal and hepatic hydatid disease causing major bile duct destruction, Journal of Surgical Case Reports, Volume 2012, Issue 4, April 2012, Page 6, https://doi.org/10.1093/jscr/2012.4.6
Close - Share Icon Share
Abstract
Echinococcosis is endemic in Mediterranean regions and is found primarily in the liver. Biliary fistula is a common complication, but major biliary duct involvement is very rare, and occurs in 0.47% of patients with hepatic hydatid disease. Cyst rupture causing secondary peritoneal hydatidosis is a rare but serious complication. We report the case of a 27-year-old man with multiple peritoneal and hepatic hydatid cysts. The patient came to our attention with cholestatic jaundice. Imaging exams showed numerous peritoneal cysts and massive hydatid disease of the liver, which involved the hepatic confluence, with destruction of the right hepatic duct and fistula formation to the left hepatic duct. The patient was treated with pre-operative albendazole therapy and radical surgery, which consisted of resection of all peritoneal cysts and extended right hepatectomy with biliary reconstruction. No recurrence was seen on CT investigations on the 12th month following surgery. Radical surgical approach remains the treatment of choice.
INTRODUCTION
Hydatid disease is a zoonotic infection caused by the larval forms of tapeworms of the genus Echinococcus, largely Echinococcus granulosus, and is endemic in Mediterranean regions, South Africa, South America and the Middle East (1,2). The liver is the most commonly involved organ, followed by the lungs and other unusual locations (1,2,3,4). Biliary fistula is a common complication, but major biliary duct involvement is very rare, and occurs in 0.47% of patients with hepatic hydatid disease (5). Cyst rupture into the peritoneal cavity is a rare but serious complication. Anaphylaxis or sudden death has been reported (1,4,6). Otherwise rupture into the peritoneum could be silent, which is unusual, and diagnosis can be made several years later with a disseminated peritoneal hydatidosis (7,8).
CASE REPORT
A 27-year-old male was referred to our surgical department with cholestatic jaundice, pruritus, acholic stools and bilirrubinuria, associated with weight loss, nausea and vomiting. Physical examination revealed jaundice, sclera icterus and mild abdominal tenderness over the right upper quadrant with an enlarged liver. There was no medical history of note and no history of blunt trauma. He had contact with dogs as a child.
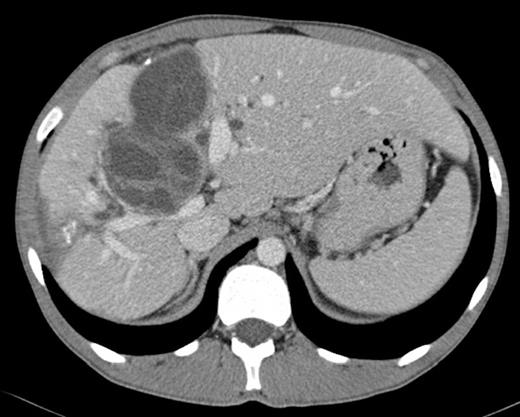
Abdominal CT scan: multiple hydatid cysts in the right lobe of the liver, one of them near the hepatic confluence

Laboratory investigations showed a slight anaemia, elevation of serum bilirrubin (conjugated 10.6 mg/dl), alkaline phosphatase (959 U/L), gamma-glutamyl transpeptidase (755 U/L). Hydatid serology was positive. Abdominal ultrasound demonstrated multiple cystic lesions spread in the liver, splenic hilum and peritoneal cavity. CT-scan confirmed the presence of numerous hydatid cysts, in different stages of development (type I-IV of Gharbi Classification), ranging from 3 to 8 cm in diameter, with 3 involving the right lobe of the liver and segment 4 (Fig.1). The splenic hilum contained a 4 cm cyst, and 9 more cysts were described in peritoneal cavity: near the gallbladder, in the root of the mesentery, in the right iliac fossa and in the Douglas pouch (Fig. 2). Cholangio pancreatography (MRCP) showed intra-hepatic bile ducts dilatation. Cholangiography (ERCP) was attempted without success. Pre-operative albendazole therapy (10 mg/Kg) was prescribed for 4 weeks.
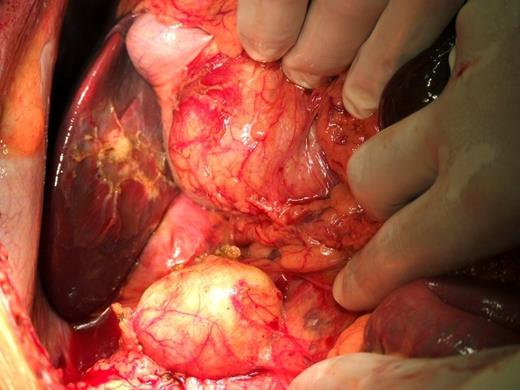

Surgical exploration confirmed the numerous peritoneal hydatid cysts and identified more lesions in the larger omentum (ranging from 3-12 cm) (Fig. 3). They were all resected, and a splenectomy was performed to remove completely the hilum cyst (Fig.4). Hydatid disease of the liver was massive, except in segments 1, 2 and 3. A cyst developing in segment 7 (7 cm) invaded the diaphragm and another voluminous cyst of 12 cm occupied the entire segment 8. A cyst of 8 cm in segments 4 and 5 involved the hepatic confluence, with destruction of the right hepatic duct and promoting a major biliary fistula with the left hepatic duct, confirmed by intra-operative transcystic cholangiography. The left hepatic duct near the hilar plate was included in the pericystic wall near segment 3. This cyst was chemically inactivated using iodopovidone (20 minutes), evacuated and followed by a thorough exploration of the cavity, which showed multiple biliary fistulae from the right sectorial hepatic ducts and a large defect in the left hepatic duct (Fig. 5). An extended right hepatectomy (segments 4 – 8), partial resection of the diaphragm and partial resection of the left hepatic duct including the fistula was performed. Reconstruction of biliary continuity was assured by a hepaticocholedocostomy, over a T-tube (Fig. 6). Confirmation of sectorial left hepatic ducts patency was done by intra-operative cholangiography.

Hepatic hydatid cyst in segments 4 and 5, after inactivation and evacuation, involving the hepatic confluence, with total destruction of the right hepatic duct and fistula formation to the left hepatic duct.

Postoperatively, he developed a left subphrenic biloma treated by CT-guided percutaneous drainage, and he was discharged on the 28th postoperative day. Albendazole was continued for 12 more weeks. T-tube colangiography on 60th day showed no extravasation of contrast or filling defect and the tube was subsequently removed. At 12 months follow up, no recurrence was seen on CT investigations.
DISCUSSION
The clinical manifestations of cystic echinococcosis are variable and are determined by the localization, size and condition of the cysts (1). Jaundice is usually associated with rupture of hepatic cysts into the biliary tract. In this particular case jaundice was due to involvement of the hepatic confluence with destruction of the right hepatic duct. The complexity and severity of this exceptional lesion requires uncommon approach, justifying our option for radical resection. Biliary continuity was assured by a hepaticocholedocostomy, over a T-tube. Spontaneous rupture of the hepatic hydatid cyst into peritoneum without any symptom is unusual (8). Our patient had no history of abdominal pain.
Ideal therapy should eliminate the parasite with low morbidity and no mortality, avoiding local recurrence. Surgery remains the gold standard treatment for hydatid disease (1-3,6,8). In case of several cysts, removal of all cysts in the same intervention is indicated (7). Radical surgery is associated with low recurrence rate and cavity-related complications, when compared with conservative approaches (2,6)
In conclusion, hydatid disease should be included in the differential diagnosis of bile duct obstruction, especially in endemic countries. Surgical removal of intact hydatid cysts, when possible, remains the treatment of choice, leading immediately to complete cure (1).



