-
PDF
- Split View
-
Views
-
Cite
Cite
N Bhardwaj, G Garcea, DM Lloyd, A rare case of multi-focal angiomyolipoma affecting the pancreas and liver, Journal of Surgical Case Reports, Volume 2012, Issue 4, April 2012, Page 5, https://doi.org/10.1093/jscr/2012.4.5
Close - Share Icon Share
Abstract
Angiomyolipoma (AML) are benign tumours composed of varying amounts of thick-walled dysplastic blood vessels, smooth muscle and mature adipose tissue derived from epithelioid cells. We present a previously unreported occurrence of multi-focal pancreatic and hepatic AMLs in a patient and discuss the diagnostic and management difficulties associated with this rare disease. In addition relevant case studies are also reviewed.
INTRODUCTION
Angiomyolipoma (AML) are benign tumours composed of varying amounts of thick-walled dysplastic blood vessels, smooth muscle and mature adipose tissue derived from epithelioid cells. They are the commonest benign tumours found in the kidney and can be associated with tuberous sclerosis complex, although the majority occur sporadically (1,2). Primary AML of the pancreas (3) and liver (4) have been described before, however there are no cases of multifocal AML involving the liver and pancreas reported in the literature.
CASE REPORT
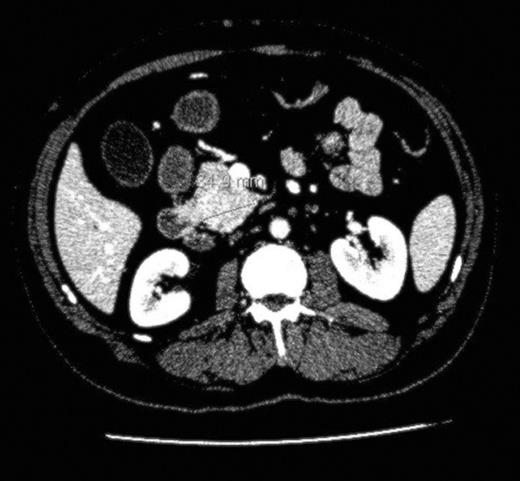
We report the case of a 61 year old man, previously treated for follicular lymphoma in the left groin with radiotherapy, presentING to our hepatobiliary department with painless obstructive jaundice ALP 592 iu/L (40-130), ALT 86 iu/L (2-53) and Bil 180 (3-17). His CA19.9 was 156 u/l and there was no clinical evidence of tuberous sclerosis. Cross-sectional imaging in the form of a CT and MRI scan reported multiple suspicious lesions in the liver (Fig. 1) and a small lesion in the uncinate process of the pancreas (Fig. 2) causing intrahepatic and common bile duct dilatation. The radiological diagnosis at this point was of a metastatic (and hence inoperable) pancreatic cancer. He underwent an ERCP and insertion of a CBD stent to relieve his jaundice and an attempted percutaneous biopsy of his pancreatic mass yielded inadequate cells. He then underwent a laparoscopy and attempted biopsy of his pancreatic and/or liver lesions. The pancreatic mass was difficult to visualise on intraoperative ultrasound however one of the liver lesions was biopsied and this was reported as an angiomyolipoma.
After re-discussion at our multi-disciplinary meeting it was felt that on balance the liver lesions were an incidental finding and in view of his age, presentation and imaging he most likely had a small pancreatic carcinoma. He underwent a pancreaticoduodenectomy and made an uneventful recovery. Histological analysis of the specimen revealed a small completely excised angiomyolipoma. Several months after his operation, he was admitted with vague abdominal pain, which resolved spontaneously. However, a CT scan performed during his admission revealed several intra-hepatic lesions of varying sizes and a growth of the original segment VI lesion. A percutaneous biopsy of one of the new lesions once again confirmed AML.
DISCUSSION
This is an unusual case for several reasons. Firstly, pancreatic AML is extremely rare, with only one case reported in the literature (3). Secondly, we believe this is the only reported case of multifocal AML affecting the pancreas and liver. There are two cases in the literature describing multi-focal AML, one involving the lung and liver (2) and the other involving the pancreas and right kidney (5). Thirdly, multiple hepatic AMLs not associated with tuberous sclerosis are rare and only a handful of cases have been reported in the past (6).
Angiomyolipomas are considered to be benign in nature although there have been a few reported cases of excised renal (7) and hepatic (8) AMLs, uncharacteristically displaying malignant potential as evidenced by their immunoreactivity to p53 on pathological analysis (which was positive in this specimen). There still remains a scarcity of data describing their natural progression and behaviour and this often makes surgical management of these lesions difficult. In this case, the pancreatic lesion was small and the consensus opinion was to treat this as a carcinoma, a reasonable assumption considering the clinical presentation and imaging results in a relatively fit 61 year old.
The next dilemma facing our team is how to deal with his enlarging hepatic AMLs. The clinical differential of hepatic AML includes lipoma, haemangioma, focal nodular hyperplasia hepatocellular carcinoma and hepatic adenoma. Although change of size in renal AMLs is a well described phenomenon (9), it is a relatively rare occurrence in the case of hepatic AMLs (10). We have decided to follow-up this gentleman with serial 6-monthly MRI scans; however this is based on anecdotal rather than robust clinical evidence.
In hindsight, although the patient underwent major surgery for a benign tumour, it is difficult to see how this could have been prevented by any further pre-operative investigations. Endoscopic ultrasound with biopsy of the lesion may have been of value in obtaining a preoperative tissue diagnosis of the primary pancreatic lesions. However, for a fit patient with a potentially resectable pancreatic tumour (on cross-sectional imaging) we believe it to be best practice to proceed to resection in the absence of definitive preoperative or intraoperative confirmation of malignancy. This remains a consensus view followed by many other pancreatic units worldwide.
We have described a fascinating and rare case of multifocal angiomyolipoma, however there are still questions regarding the ideal management of patients with these lesions, particularly those growing in size in the liver. Reporting of such cases is essential to further delineate the natural history of this pathology.



