-
PDF
- Split View
-
Views
-
Cite
Cite
S Gupta, S Garg, R Agarwal, R Sen, Aspiration cytology of adenomatoid tumor of epididymis: An important diagnostic tool, Journal of Surgical Case Reports, Volume 2012, Issue 4, April 2012, Page 11, https://doi.org/10.1093/jscr/2012.4.11
Close - Share Icon Share
Abstract
Adenomatoid tumor is a benign mesothelial neoplasm of the paratesticular region in males but can also occur in female genital tracts. The epididymis is the most common site of involvement and constitutes 32% of paratesticular neoplasms.
We diagnosed a case of adenomatoid tumor on cytopathology in 24 years old male, who presented with mass lesion right epididymis since 2 months. The diagnosis was confirmed on histopathology and immunohistochemistry after surgical excision of the nodule.
FNAC is a rapid, reliable and cost effective diagnostic tool for preoperative diagnosis to take appropriate surgical decisions. Pathologists should be aware of the cytological features of such lesions so as to differentiate it from other paratesticular lesions.
INTRODUCTION
Adenomatoid tumor is a benign neoplasm of mesothelial origin (1). It is a common tumor of male paratesticular tissues (epididymis, tunica or spermatic cord) and has also been described in females (uterus, fallopian tube, ovary and paraovarian tissues). The majority of these tumors are asymptomatic and presents as a mass in the genital area, which is worrisome to both patient and clinician and requires a definitive diagnosis to rule out malignancy (2). FNAC is a rapid, reliable and cost effective diagnostic tool for preoperative diagnosis of paratesticular swellings.
We report a case of epididymal adenomatoid tumor diagnosed on aspiration cytology, which was confirmed on histopathology and immunohistochemistry.
CASE REPORT
A 24 year old male presented with progressively increasing painless swelling of the right epididymis for 2 months. There was no history of trauma. His past and personal history was not significant. Local examination revealed a firm, mobile, mildly tender mass measuring 1.5x1.5cm in diameter in the right epididymis. Testes were normal bilaterally. Clinically, a diagnosis of epididymal cyst was made. Routine hematological and biochemical tests were within normal limits. Ultrasonography of the swelling revealed a well-defined hypoechoic lesion of 18x11mm, with increased flow on color Doppler (Figure 1).

Scrotal ultrasonography. Well defined hypoechoic lesion of size 18x11mm in right epididymis (white arrow) and normal right testis (black arrow)
Fine needle aspiration of the swelling was performed using a 23-gauge needle and 10 ml syringe. FNA yielded scanty, whitish aspirate mixed with blood. Smears were stained with Romanosky and papanicolaou stain. Examination of the smears revealed cells arranged in loose aggregates in a vaguely glandular pattern and singly scattered at places along with stromal fragments and a few inflammatory cells in a haemorrhagic background. The cells have ovoid, vesicular nuclei, finely granular and evenly distributed chromatin, small nucleoli and abundant cytoplasm with vacuolization at places (Figure 2).
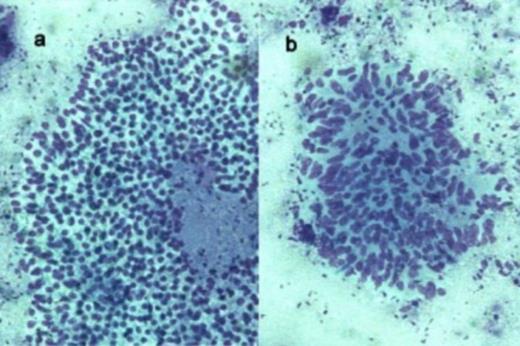
Photomicrograph of FNAC smears showing a). monolayered sheets of cells with indistinct cells borders and pale vacuolated cytoplasm b). stromal cells (Romanowsky x 200)
The patient underwent a conservative testis sparing surgery with the excision of epididymal nodule. The nodule measured 1.5x1.2cm in diameter and the cut section was gray-white. Histopathology revealed some slit like or glandular spaces lined by flattened cells with intracytoplasmic vacuoles in an abundant fibromuscular stroma and few inflammatory cells. On immunohistochemistry tumor cells were positive for mesothelial marker calretinin and negative for CD34, factor-VIII and CEA. The final diagnosis of adenomatoid tumor was made (Figure 3).
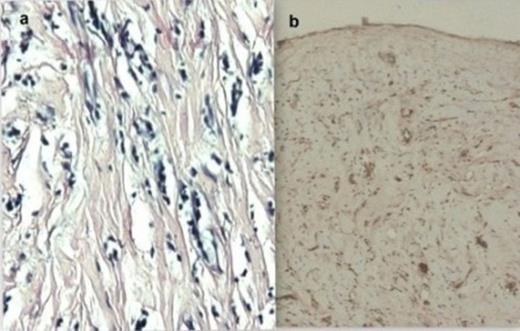
Photomicrograph showing a) Histopathological features of adenomatoid tumor consisting of dilated tubular structures lined by cuboidal to flattened epithelial cells (H and E x 200). b) Immunohistochemical positivity for calretinin (IHC x 100)
DISCUSSION
Adenomatoid tumor(AT). is the most common benign tumor of paratesticular tissue and accounts for 32% of all tumors in this location (3). The term adenomatoid tumor was first coined by Godman and Ash in 1945 (4,5). Besides the epididymis, adenomatoid tumor can be located in the spermatic cord, prostrate, ejaculatory ducts and scrotal capes and in females it can be located in uterus, fallopian tubes and ovaries (6). It is common in the 3rd and 4th decades of life (4,6,7). Most of these are asymptomatic and are noticed incidentally by the patient or by the physician on physical examination, as a painless intrascrotal mass. It presents as a relatively small, well demarcated uncapsulated nodule, usually less than 2cm in diameter. The largest diameter reported is 12cm. (6,7).
The histogenesis of AT has been a matter of debate for many years with the proposed cells of origin being endothelial, mesothelial, mesonephric, mullerian and epithelial (8). Though the structural and immunohistochemical studies support the mesothelial origin, the usual coexistence of chronic inflammatory cells and fibrosis suggests mesothelial hyperplasia (6,8).
The first cytological description of AT was described by Perez-Guillemro et al in 1989 (2). Adenomatoid tumors have been described briefly in textbooks on FNA cytology and only a few cases of this entity diagnosed by FNAC are recorded in the literature (2,5).
On fine needle aspiration cytology adenomatoid tumors reveal abundant cellularity and comprise sheets and multilayered clusters of monotonous cells with round or ovoid, eccentric nuclei containing small central nucleoli. Paranuclear clearing with a pink colouration (giemsa stain). or a clear vacuole like area (papanicolaou stain) with a background of naked nuclei and stromal fragments (2). The cytological differential diagnosis include reactive mesothelial hyperplasia, papillary cystadenoma, spermatic granuloma, malignant mesothelioma and metastatic adenocarcinoma (4,5).
Reactive mesothelial cells with hyperplasia can be seen in hydrocoele fluid, The cells show anisocytosis and pleomorphism and have a moderate amount of pale cytoplasm. Nuclear grooves, lobulation and mitosis can be seen. They may not have definite arrangement of cells, a feature seen distinctly in adenomatoid tumors. Cytologically papillary cystadenoma comprises of papillary structures and single isolated cells without nuclear atypia and with cytoplasmic vacuoles in a mucoid background. Malignant mesothelioma show a diffuse cell pattern with cells having ruffled borders with dense cytoplasm, nuclear enlargement, macronucleation and multinucleation. Spermatic granuloma shows histiocytes filled with sperm heads and debris in the background. Metastatic adenocarcinoma show cytological features of malignancy and cells are positive for mucicarmine (4,5).
On histopathology, the tumor has a plethora of microscopic appearances, with proliferation of cells ranging from cuboidal to flattened, which forms solid cords with an epithelial appearance alternating with channels having dilated lumina simulating vascular structures. The prominent intervening stroma may contain abundant smooth muscles and elastic fibres; it may also have a reactive desmoplastic quality and be infiltrated by inflammatory cells. The tumor cells may exhibit prominent cytoplasmic vacuolization. On immunohistochemistry these cells are positive for mesothelial related markers ( calretinin, HMBE1). and negative for CEA and factor VIII related antigen (6,7).
Ultrasonography along with cytological features helps to make a definite diagnosis and to evolve an organ sparing surgical approach (4).
The clinicocytologic presentation of AT is unique and easily recognized by FNA cytology. The preoperative cytology may be used as an important diagnostic tool to evaluate the paratesticular masses. Pathologist should be aware of cytological features of these common lesions to avoid aggressive or unnecessary surgical procedures.



