-
PDF
- Split View
-
Views
-
Cite
Cite
ID Goukassian, SR Kussman, Y Toribo, DB McAneny, JE Rosen, A rare case of non-metastatic cholangiocarcinoma in a long standing choledochal cyst, Journal of Surgical Case Reports, Volume 2012, Issue 4, April 2012, Page 12, https://doi.org/10.1093/jscr/2012.4.12
Close - Share Icon Share
Abstract
Choledochal cysts are rare benign growths that can develop into cancerous lesions if left untreated. The cysts are commonly discovered incidentally during imaging procedures for other reasons. Surgical resection is recommended to avoid risk of cancer or metastatic disease. A rare case of a non-metastatic cholangiocarcinoma in a longstanding choledochal cyst is presented in this case report.
INTRODUCTION
Choledochal cysts are rare benign cysts originating in the biliary tree historically prevalent in children, females and the Japanese population. Incidence of cyst disease varies from as common as 1 in every 13,000 to 1 in 2 million (1). The longer these cysts remain in place and are allowed to grow, the higher the risk of developing a malignancy. Here we present a case report of a 26 year old female with a long standing cholangiocarcinoma in a longstanding choledochal cyst.
CASE REPORT
A case of cholangiocarcinoma in an unresected choledochal cyst with local invasion into pancreas and lack of nodal involvement in a total of 10 resected lymph nodes is presented. A 26 year old female presented to our surgical oncology clinic for evaluation of a Type I choledochal cyst. The cyst was identified incidentally by ultrasound seven years prior during the patient’s first pregnancy. A computed tomography (CT) scan demonstrated a 3cm X 8 cm dilated bile duct. A magnetic resonance cholangiopancreatogram (MRCP) was performed and demonstrated a fusiform dilation of the extrahepatic common bile duct measuring at least 7.4 x 4.8 x 6.2 centimeters and enhancing soft tissue polypoid mass arising from the medial wall of the cyst that is concerning for malignancy but no sign of metastatic disease (see figure 1). Resection was recommended at the time but patient opted to monitor growth and delayed surgery. She denied jaundice, acholic stools, vomiting, nausea or fever but did report occasional left upper quadrant pain. A repeat MRI (magnetic resonance image) in 2011 demonstrated a seven centimeter fusiform choledochal cyst abutting the pancreas with an aberrant pancreatic duct and a concerning solid component at the anteriomedial aspect of the cyst. There was no evidence of adenopathy or infiltration of surrounding tissue.
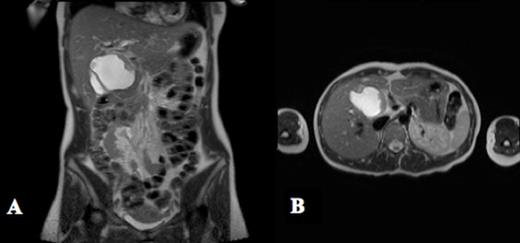
MRCP shows a fusiform dilation of the extrahepatic common bile duct measuring 7.4 x 4.8 x 6.2 cm in the axial (A) and transverse planes (B). There is an enhancing soft tissue mass with a thickness of 1.1 cm protruding into the lumen of the cyst that is concerning for malignancy
She underwent a trans-abdominal resection of choledochal cyst with Roux-en Y hepaticojejunostomy, open cholecystectomy and liver biopsy. No malignancy was identified in the liver. The cyst measured seven centimeters at largest diameter and was classified as Type I Ib (a choledochal cyst with focal dilation of extra hepatic biliary tree). The patient did not have any postoperative complications and was discharged on postoperative day four.
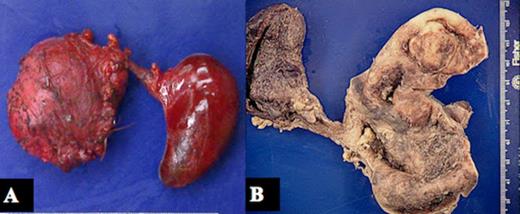
Gross image of choledochal cyst and gallbladder. A shows unopened specimen with cyst on left and gallbladder on right. B shows dissected cyst on right and gallbladder on left.
Figure 2 demonstrates the cyst before and after sectioning. Final pathology results revealed an adenocarcinoma with focal squamous differentiation (see figure 3). The tumor was classified as pT3 as the pancreas had focal invasion with negative margins. Ten lymph nodes were resected and all were negative for metastasis (N0). As she had no evidence of metastatic disease, her AJCC stage was pT3N0M0 (Stage IIA). She was enrolled into a Phase II clinical trial for chemotherapy and mindfulness relaxation which includes four cycles of gemcitabine/ capecitabine followed by radiotherapy with concurrent capecitabine. She was asymptomatic at last follow up visit.
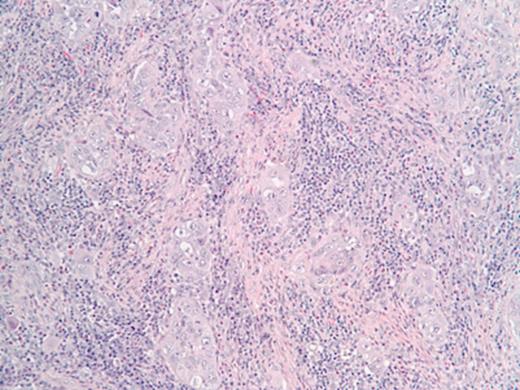
H&E stain (x 200) demonstrates poorly differentiated adenonocarcinoma with focal squamous changes.
DISCUSSION
Cholangiocarcinoma is a complication of choledochal cysts due to chronic mucosal irritation and the risk is increased if prior drainage procedures performed prior to cyst excision (2). While the most common presentation has been in female infants in the past, more disease is being reported in individuals 18 and older. There is no clear etiology of the disease in adults but an anomalous junction between the bile duct and pancreatic duct is a common finding (2). Choledochal cysts that go untreated increase the risk of harboring a cholangiocarcinoma (1). Children usually present with a triad of symptoms- jaundice, abdominal mass and pain. In comparison, adults often present with abdominal pain and are thought to have pancreatitis or biliary tract symptoms and diagnosis is often delayed due to nonspecific and intermittent symptomatology (3). Preferred treatment for both groups is excision of the cyst and biliary reconstruction (1). Drainage of the cysts is no longer preferred due to reports of complications (4). The standard treatment for Type I choledochal cysts is total excision in part, due to the possibility of carcinoma developing in the cyst and in part to avoid stricture formation (4-6). The percentage of patients found to have cholangiocarcinoma after excision varies from 9.7% to 25%, strongly supporting that complete and aggressive resection is warranted (3).
The most common cysts in adults are Type I cysts (dilation of extrahepatic bilary tree) followed by Type IV (dilations of intrahepatic and extrahepatic biliary tree) (1). While the surgical treatment may differ based on the type of cyst, no specific cysts type has been reported to indicate a higher risk of developing into cancer. Mortality from surgery is very rare in adult patients. If left untreated, the risk malignant transformation increases proportionally with the time elapsed since initial choledochal cyst diagnosis (7). Edil et al reported the largest series of choledochal cyst in North America; out of 73 adults, 4 harbored malignancy with two having cholangiocarcinoma with tumors smaller than 5 centimeters. Of these two, one had lymph node involvement while the other did not (8).
Of the few cases of choledochal cyst excision that have been reported in pregnant women, elective caesarian sections were performed to avoid stress and possible complications that the cyst could cause during labor and vaginal birth (9). Our patient’s cyst was discovered incidentally during her first pregnancy and she opted to wait to have it removed afterwards and had another child before having this cyst removed. However, no complications associated with her cyst were reported during either of her pregnancies.
In addition to complete resection, treatment options include radiotherapy and chemotherapy. In recent years, gemcitabine-based chemotherapy has had positive effects on improving the rate of survival in more advanced cases of cholangiocarcinoma (10). Currently, there are clinical trials aimed at investigating the effectiveness of gemcitabine in combination with other therapeutic agents and our patient is enrolled in such a trial.



