-
PDF
- Split View
-
Views
-
Cite
Cite
N Simion, Alithiasic cholecystitis treated by percutaneous cholecystostomy in a patient with severe septic shock and neutropenia, Journal of Surgical Case Reports, Volume 2012, Issue 2, February 2012, Page 4, https://doi.org/10.1093/jscr/2012.2.4
Close - Share Icon Share
Abstract
Acalculous cholecystitis is a relatively rare form of cholecystitis appearing in severely ill patients. We chose the case of a young patient under chemotherapy for myeloid leukaemia who developed a severe septic shock secondary to an alithiasic cholecystitis. Because of hemodynamic instability needing high-dose of vasoactive amines, percutaneous gallbladder drainage was done. After this intervention, the septic shock could be controlled, but a bleeding liver laceration was observed, fortunately without morbidity consequences.
Abdominal infections are life-threatening complications in neutropenic patients. Neutropenic enterocolitis is the most important entity, but the acute cholecystitis, even rarer, had been described in several reports, suggesting that this infection could represent a difficult trap.
INTRODUCTION
Patients with leukaemia undergoing aggressive chemotherapy are often affected by abdominal infections becoming life-threatening conditions. It is a diagnostic challenge for the physician to detect the cause of abdominal symptoms (infectious and non-infectious) in these patients (1,2).
Acalculous cholecystitis is a form of acute cholecystitis seen more frequently in immunosuppressed and high risk patients. The treatment of choice for acute cholecystitis is surgical, but in selected cases conservative treatment followed by elective cholecystectomy later or cholecystostomy could represent an alternative (2,3).
CASE REPORT
We report the case of a 36-year-old man with the diagnosis of acute myeloid leukemia type M4 (>90% blasts). The patient was treated firstly by cytoreduction chemotherapy followed by induction chemotherapy (cytarabine + idarubicine). During this period the patient was admitted in hospital with diarrhoea and febrile agranulocytosis. Neutropenic colitis was diagnosed and confirmed by CT scan, the patient being treated with broad spectrum antibiotics leading to a good recovery.
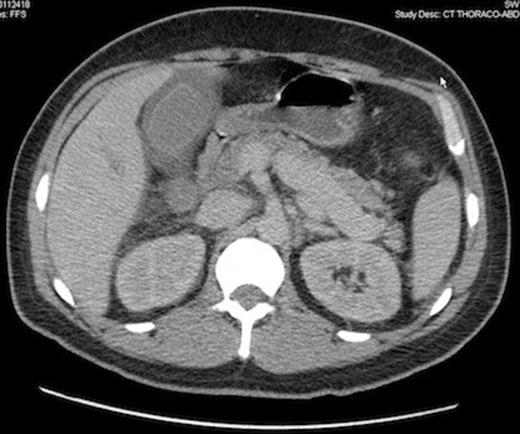
Computed tomography scan demonstrating gallbladder wall thickening and pericholecystic liquid, without gallbladder lithiasis, confirmed by ultrasonography.
One month later the first consolidation chemotherapy (cytarabine + amsacrine) was done and 6 days afterwards the patient presented diarrhoea without abdominal pain or fever. The laboratory investigations revealed a total leukocyte count of 500/mm3, a haemoglobin level of 68 g/L and a platelet count of 11 000/mm3. Despite supportive treatment and antibiotics for a supposed improving colitis, the patient complained of right upper quadrant abdominal pain, high fever (40°C) and hypotension needing ICU admission with the diagnose of abdominal sepsis. A positive Murphy’s sign was observed at physical abdominal examination. The radiological imaging was suggestive for an alithiasic cholecystitis, even though a transverse colon wall thickening was also seen in computed tomography.
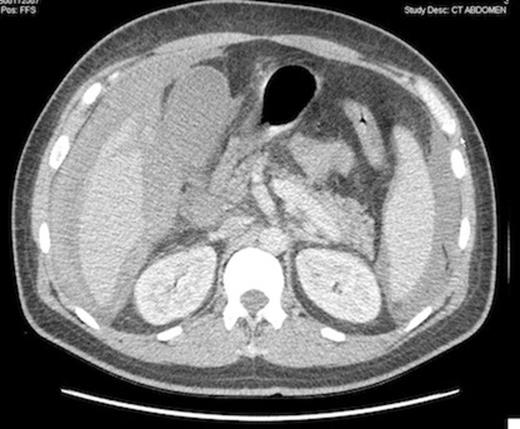
Computed tomography scan showing peritoneal bleeding from hepatic laceration after gallbladder percutaneous transhepatic drainage.
The patient was considered to unstable for a surgical intervention and an emergency percutaneous CT-guided cholecystostomy was done, in spite of a very low platelet count (7 000/mm3). 24 hours later, the septic shock rapidly improved, but hemoglobin level fell down from 83 to 61 g/L. A CT scan showed a bleeding liver laceration with intraperitoneal haemorrhage secondary to the transhepatic percutaneous gallbladder drainage.
The patient was treated conservatively receiving several transfusions and went well without any further complications.
DISCUSSION
Alithiasic cholecystitis is an entity occurring typical in the elderly, severely ill and high risk patients typically hospitalised in the ICU. The frequency of acute cholecystitis between patients with myelosupressive chemotherapy and neutropenia is estimated at 0.4% in the literature, with a nearly 30% mortality. The majority of the neutropenic patients develop acalculous cholecystitis, in contrast with non-neutropenic patients to whom acalculous cholecystitis comprises only approximately 5% of all cases of acute cholecystitis (1).
The clinical diagnosis of acute cholecystitis (AC) remains difficult in the patient population with multiple comorbid conditions, the typical signs and symptoms being easily masked among ventilated, paralyzed or immunosuppressed patients. Ultrasound is an established valuable imaging method if cholecystitis is suspected and a thickened gallbladder wall greater than 3mm is considered typical for diagnosis. Other frequent sonographic findings are pericholecystic fluid and over-distension. Similar findings can be demonstrated by CT, computed tomography being extremely useful in the assessment of septic shock of unknown origin in this patient population (1,4).
Laparoscopic cholecystectomy is widely considered as the treatment of choice for acute cholecystitis and it can be performed safely in selected patients. Surgery in patients with neutropenia, thrombopenia and sepsis who present with an acute abdomen is however associated with a high mortality. Percutaneous cholecystostomy (PC) was described as a minimally invasive, image-guided procedure and has become an alternative treatment strategy for high-risk patients with acute calculous or acalculous cholecystitis who are unfit for urgent surgery (1,5).
Percutaneous cholecystostomy could be also used as a method of exclusion of the gallbladder/biliary tree as a source of sepsis in unstable severely ill patients. The positive response is defined as resolution of right upper quadrant abdominal pain and normalization of general clinical state, usually within 48 hours (4).
The procedure can be performed CT-guided or US-guided, even at the bedside in the ICU. The safety of the procedure and its minimal invasiveness made it a valid treatment option for a patient not responding to antibiotic therapy or being in severe shock and unfit for immediate cholecystectomy. The results from several series prove that the percutaneous gallbladder drainage is safe and that it was effective in more than 85% of the patients. There were no bile duct injuries or any other major surgical complications in this group of patients (6,7).



