-
PDF
- Split View
-
Views
-
Cite
Cite
Bonnie H. Wang, Vincent Pureza, Huan Wang, A tale of Wünderlich syndrome, Journal of Surgical Case Reports, Volume 2012, Issue 11, November 2012, rjs015, https://doi.org/10.1093/jscr/rjs015
Close - Share Icon Share
Abstract
Wunderlich syndrome is a rare entity characterized by acute onset of spontaneous, non-traumatic renal hemorrhage into the subcapsular and perirenal spaces. It can be fatal if not promptly recognized clinically and treated aggressively. We report a case of a 63-year-old Caucasian female who was presented to the emergency department with acute onset of sharp abdominal and right flank pain, and hypotension. An urgent abdominal and pelvic computed tomography scan with contrast demonstrated a large (13 × 12 × 8.5 cm) right perinephric hematoma of unknown etiology. The patient subsequently underwent renal angiogram that demonstrated active extravasation of the right superior renal artery. She underwent successful embolization procedure and responded well to fluid resuscitation. She remained hemodynamically stable and was discharged home without further events.
INTRODUCTION
Wunderlich syndrome (WS) is a rare condition in which spontaneous renal hemorrhage occurs into the subcapsular and perirenal spaces. It can manifest with a life-threatening presentation of fulminant hypovolemic shock. This condition was first observed by Bonet in 1700, and was first described clinically as ‘spontaneous renal capsule apoplexy’ by Wunderlich in 1856 [1, 2]. Coenen first used the term WS in 1910 [1, 2].
The most frequently associated etiologies include benign and malignant renal tumors, such as renal angiomyolipoma and renal cell carcinoma, vascular lesions such as polyarteritis nodosa and renal infection. Renal cysts, blood dyscrasias or anticoagulant and antiplatelet therapy are some of the less common causes. It is classically associated with pain in the flank, a palpable abdominal mass and hypovolemic shock (Lenk's triad). A computed tomography (CT) scan is the diagnostic modality of choice. Management is mainly expectant, although endovascular embolization or urgent surgical intervention (nephrectomy or evacuation of hematoma) may be required in cases of massive hemorrhage. We report a case of WS in a 63-year-old female who presented with spontaneous perinephric and subcapsular hemorrhage from the superior right renal artery.
CASE REPORT
A 63-year-old Caucasian female with no known history of trauma, anticoagulation or bleeding diathesis was presented to the emergency department with sudden-onset, sharp abdominal and right flank pain. The associated symptoms included near-syncope, diaphoresis, nausea and vomiting. Her personal history included renal calculus, hypertension and diabetes mellitus. Previous surgical history included back surgery for hemagioblastoma removal years ago, but she denied history of percutaneous nephrolithotomy. She claimed no known drug allergies and no recent changes in home medications.
Although persistently hypotensive at her initial presentation, she later developed hemodynamic instability systolic blood pressure of 82 mmHg. She was stabilized with crystalloid fluid resuscitation without additional needs for blood products. A physical examination revealed a mildly obese, afebrile female with severe right upper quadrant, epigastric and costovertebral angle tenderness.
The patient's hemoglobin was 10.5 g/dl, creatinine 1.39 mg/dl, estimated glomerular filtration rate 38 ml/min/1.73 m2 and international normalized ratio of 1.1.
A pre- and post-contrast CT scan of the abdomen and pelvis revealed a large right perinephric hematoma within the anterior aspect of the retroperitoneum (Fig. 1). This hematoma distended the renal fascia, crossed the midline and displaced other peritoneal and retroperitoneal structures. Free fluid and a hyperdense focus of vascular contrast were present adjacent to the hematoma. The estimated size of the hematoma was 13 cm in the cephalocaudad, 12 cm in the transverse and 8.5 cm in the anteroposterior dimension. The vena cava, renal artery and renal vein were narrowed likely due to vasospasm, but the aorta was otherwise unremarkable.

Peri- and paranephric hematoma filling the right retroperitoneum. Pre-contrast and contrast enhanced abdominal and pelvic CT with (A) axial, and (B and C) coronal views. The hematoma distends the renal fascia, crosses the midline and displaces other peritoneal and retroperitoneal structures. Free fluid, and a hyperdense focus of vascular contrast is present adjacent to the hematoma (best seen in A). An incidental ∼18 mm right lower pole renal calcification (B). The estimated size of the hematoma was 13 × 12 × 8.5 cm. Incidental finding of cholelithiasis (C)
An emergent renal angiogram revealed two right renal arteries with active contrast extravasation from the subsegmental branch of the superior right renal artery (Fig. 2A). This was successfully embolized (Fig. 2B). This case was clinically diagnosed as a spontaneous retroperitoneal hemorrhage with subcapsular hematoma, otherwise known as WS.
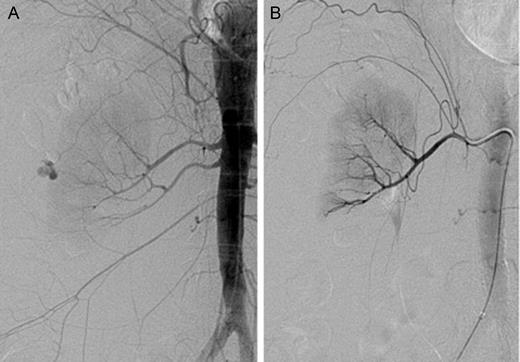
Identification and subsequent embolization of an active extravasation from the superior right renal artery. (A) Renal angiogram of the right kidney prior to embolization. Both a superior and an inferior right renal arteries are present. There is an active extravasation of blood from the subsegmental branch of the superior right renal artery. (B) Post-embolization renal angiogram. There is no definitive focus of active extravasation
A follow-up abdomen/pelvis CT/CTA demonstrated complete resolution of active extravasation and no pseudoaneurysm formation. The patient remained hemodynamically stable and was discharged home uneventfully. Her 3-month follow-up magnetic resonance imaging (MRI) did not reveal any remarkable findings.
DISCUSSION
WS, or a spontaneous retroperitoneal hemorrhage from the kidney, was described by Carl Reinhold August Wunderlich in 1856 [1]. It is characterized by acute onset of spontaneous renal bleeding confined to the subcapsular and perirenal spaces [1, 3, 4]. It is a rare clinical phenomenon with only 250 known cases reported since 2003 [5]. The syndrome is commonly associated with various pathological conditions such as neoplasm and vascular disease [3]. Accounting for ∼60–65% of all cases, renal neoplasms are the most common cause of WS [4]. Angiomyolipoma is the most common benign neoplasm responsible for WS, while renal cell carcinoma is the most common malignant neoplasm [4]. However, the overall prevalence of WS as a complication of renal cell carcinoma occurs in only 0.3–1.4% of cases, whereas it is estimated to occur in 13–100% of cases of renal angiomyolipoma [5]. It is frequently found in conjunction with hypertension (33–50%) and atherosclerosis (80–87%) [2, 6]. In some cases, no causes can be identified [1].
WS is classically associated with acute lumbo-abdominal pain, palpable mass and general deterioration with hypovolemic shock (Lenk's triad). Clinically, however, it commonly presents with abdominal pain (67%), hematuria (40%) and hypovolemic shock (26.5%) [2, 7, 8]. A CT scan is considered the gold standard for establishing the diagnosis, and oftentimes used to elucidate the etiology for the condition [1, 4]. The main criterion for diagnosis is bleeding in the subcapsular and perirenal space [1]. A CT scan is limited, however, by the hemodynamic stability of the patient, and may miss rare cases of segmental arterial mediolysis [2, 3]. MRI is an alternative if a CT scan fails to identify an active bleeding source [4].
In our patient, although the superior renal artery was identified angiographically as the source of her spontaneous hemorrhage, the etiology has remained elusive. Most commonly, renal artery hemorrhage is post-traumatic or iatrogenic. Nonetheless, such occurrences in association with neurofibromatosis and spontaneous renal arterial rupture without identifiable causes have also been reported [9]. Because the true etiology may be obscured by the perinephretic hematoma, follow-up imaging is recommended. In this case, the 3-month follow-up MRI did not reveal any remarkable findings.
Management of WS is mainly expectant, although endovascular or surgical interventions may be required in cases of massive hemorrhage or persistent hemodynamic instability. Some urologists recommend an early or immediate exploratory surgery, with possible nephrectomy if needed. Others prefer renal arteriography with embolization as an important diagnostic and therapeutic method [1, 6, 8]. Although there are not yet evidence-based guidelines to favor either approach, transarterial embolization (TAE) has become the choice of initial treatment for renal hemorrhage, irrespective of causes [10]. TAE allows for selective embolization of the bleeding vessel(s), while sparing the normal renal tissue. It has all the advantages of a minimally invasive procedure, including a more rapid recovery, shorter hospital stay and earlier resumption of physical activity [10].
References
- hypotension
- computed tomography
- renal artery
- embolization
- emergency service, hospital
- extravasation of diagnostic and therapeutic materials
- flank pain
- european continental ancestry group
- abdomen
- pelvis
- arteriography, renal
- hematoma, perinephric
- fluid resuscitation
- causality
- symptom onset
- renal hemorrhage



