-
PDF
- Split View
-
Views
-
Cite
Cite
Duminda Subasinghe, Sivasuriya Sivaganesh, Dharmabandhu N. Samarasekera, Haemosuccus pancreaticus due to aberrant vessels from the coeliac trunk: a rare cause of Gastrointestinal (GI) bleeding with diagnostic and therapeutic challenges, Journal of Surgical Case Reports, Volume 2012, Issue 11, November 2012, rjs013, https://doi.org/10.1093/jscr/rjs013
Close - Share Icon Share
Abstract
Haemosuccus pancreaticus (HP) is a rare life-threatening cause of intermittent upper Gastrointestinal bleeding. We report the first documented case of HP due to bleeding from aberrant vessels originating from the coeliac trunk feeding the head of the pancreas. Our patient underwent initial surgery and subsequent angio-embolization. This case report describes the challenges faced during the diagnosis and treatment.
INTRODUCTION
Haemosuccus pancreaticus (HP) is a potentially life-threatening clinical entity. It is described as bleeding from the ampulla of Vater where blood comes via the pancreatic duct. It is a rare cause of intermittent upper Gastrointestinal (GI) bleeding which occurs in 1:1500 cases of GI bleeding. It was first reported in 1931 by Lower and Farrell [1] who reported bleeding from an aneurysm of the splenic artery coming via the pancreatic duct and the ampulla of Vater. To date, about 125 cases have been reported in the literature. Here, we report the first case of HP due to aberrant vessels from the coeliac trunk and the difficulties faced in the management.
CASE REPORT
A 63-year-old male who had been investigated for iron deficiency anaemia of 1 year duration presented with repeated bouts of melaena. He was a hypertensive for which he was on regular antihypertensive treatment. He did not give a past history suggestive of peptic ulcer disease, chronic pancreatitis, alcohol consumption or chronic liver disease. He was not on medications such as non-steroidal anti-inflammatory drugs or anti-coagulants. On examination, he was pale but there were no stigmata of chronic liver disease. His abdominal examination was normal except the digital examination of rectum revealing melaena stools. His haematological investigations including iron studies were suggestive of iron deficiency anaemia. The upper GI endoscopic examination showed mild antral gastritis. Colonoscopy was normal. Superior mesenteric artery angiogram showed abnormal serpiginous vessels in relation to the right colic artery. He was further investigated with capsule enteroscopy and contrast CT abdomen, but showed normal findings. Subsequently, he underwent extended right hemi-colectomy (Fig. 1). The histology of the specimen showed abnormal vessels in the serosa and subserosa of the right colon.
Two weeks later he presented again with an episode of haematemesis and haematochezia. His full blood count showed a haemoglobin of 5.5 g/dl with microcytic hypochromic anaemia. Following resuscitation and stabilization, he underwent urgent upper GI endoscopy which revealed fresh bleeding from the ampulla of Vater.
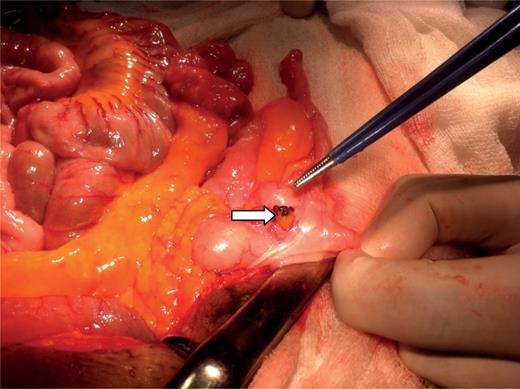
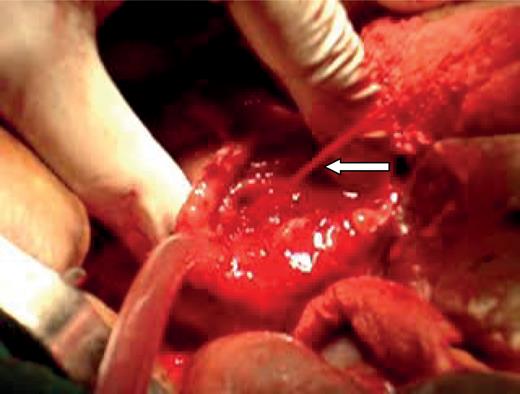
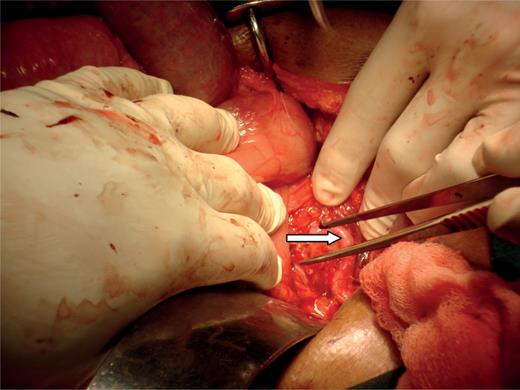
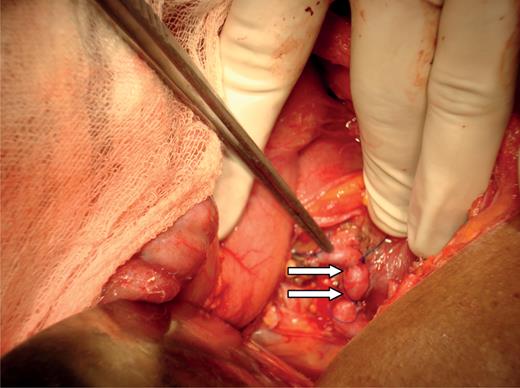
An emergency laparotomy was done to control the bleeding. A duodenotomy was done and pulsatile bleeding from the ampulla of Vater was seen (Fig. 2). On exploration, there was an abnormal tortuous vessel on the pancreatic head (Fig. 3), which was originating from the coeliac trunk entering the head of the pancreas with several branches. Abnormal vessels were ligated and haemostasis was achieved (Fig. 4). Post-operatively he also underwent angio-embolization of abnormal vessels originating from the coeliac trunk (Fig. 5) and was discharged on post-operative day 14, but subsequently presented with an episode of massive upper GI and lower GI bleeding. Repeat angio-embolization failed due to difficulties in selective embolization of aberrant vessels in the pancreatic head region. Patient did not consent for a pancreatectomy and subsequently passed away due to massive GI bleeding.

Coeliac angiogram showed aberrant vessel arising from celiac trunk.
DISCUSSION
HP is most commonly caused by a rupture of an aneurysm of the splenic artery associated with acute or chronic pancreatitis. Pseudoaneurysms of the hepatic, gastroduodenal and pancreaticoduodenal arteries have also been reported as sources of bleeding [2, 3]. Pancreatolithiasis, pseudocyst of the pancreas, trauma and rupture of primary splenic aneurysms have been identified as other uncommon causes [4–7]. According to Vimalaraj et al. [8], in a case series of 31 HP patients, they had identified the bleeding source arising from the splenic artery (n = 17), gastroduodenal artery (n = 5), superior pancreaticoduodenal artery (n = 1), inferior pancreaticoduodenal artery (n = 2) and from the superior mesenteric artery (n = 1). However, our patient had a different mechanism due to abnormal feeding vessels feeding the pancreatic head from the coeliac trunk. Also this patient had associated vascular malformations involving subserosal capillaries in the right colon. It was difficult to make the diagnosis of HP because of intermittent haemorrhage from a source that was not readily visualized by endoscopy. According to the previous authors, the management for HP should be aimed at eradicating the source of bleeding completely. There are two choices for the treatment of HP: (i) surgery (e.g. resection of the pancreas head or tail) and (ii) radiological embolization [9].
If the source of haemorrhage is found by arteriography, interventional radiological therapy should be done. Recently, Benz et al. [10] reported the interventional radiological therapy of HP by implantation of an uncoated metal Palmaz stent across the aneurysmal segment of splenic artery. For the patient with HP who has a pancreatic disease such as pancreatic pseudocyst, surgical treatment may be appropriate. However, our patient did not show any clinical or radiological features suggestive of pancreatitis. At the time of acute bleeding, we did not have the facilities for the emergency angio-embolization. Therefore, the only option for control of bleeding was emergency surgery which was successful at the time and followed by angio-embolization using gelform. Intraoperative ultrasonography is useful to confirm the origin of haemorrhage, but in our setting, we did not have facilities for intraoperative ultrasonography.
Conservative surgery by ligature of the pancreatic ducts has been used, but the results are unsatisfactory because the causal lesion remains intact. Arterial ligation is also effective, but it does not avoid the risk of recurrence. Therefore, we planned for a pancreatic resection, but the patient did not consent for this procedure.
In conclusion, there are several lessons to be learnt from this rare case. In evaluating patients with recurrent obscure GI bleeding, it is important always to remember that the pancreas is a part of the upper GI tract which is prone to be the source of haemorrhage. Also it could be a diagnostic challenge even to an expert in GI endoscopy to diagnose this condition unless there is active bleeding from the papilla at the time of endoscopy.



