-
PDF
- Split View
-
Views
-
Cite
Cite
Kristóf Dede, Ferenc Salamon, András Taller, Dániel Teknős, Attila Bursics, Autoimmune pancreatitis mimicking pancreatic tumor, Journal of Surgical Case Reports, Volume 2012, Issue 11, November 2012, rjs012, https://doi.org/10.1093/jscr/rjs012
Close - Share Icon Share
Abstract
Autoimmune pancreatitis (AIP) is a rare disease of unknown pathomechanism. It belongs to the IgG4-related disease family and responds well to steroids, although the relapse rate can reach up to 20–30%. Differentiating AIP from the more common pancreatic cancer can be very challenging. About 20% of AIP is diagnosed postoperatively during final histological examination. Each of the investigative tools can add something to the definitive diagnosis; the question remains whether it is possible to prevent an unnecessary resection. Through our case we would like to demonstrate the differential diagnostic opportunities and present the literary background of this issue. In conclusion, we can state that whenever a focal pancreatic lesion is encountered AIP should always be considered.
INTRODUCTION
There are two forms of autoimmune pancreatitis (AIP), type 1 is called ‘lymphoplasmocytic sclerosing pancreatitis’ and type 2 is the ‘idiopathic duct-centric pancreatitis’. AIP type 1 seems to be a member of the ‘IgG4-related group of diseases’, associated with high serum level of IgG4 gamma globulin fraction, IgG4-positive plasma cell tissue infiltration and sclerosis [1–4].
CASE REPORT
A 60-year-old male is presented with abdominal pain. On CT scan, a 70 × 66 × 48 mm' lesion was identified in the tail of the pancreas. Repeated aspiration demonstrated no malignancy, tumor markers were within the normal range. Control imaging studies showed enlargement of the mass, infiltrative growth, venous compression and appearance of a pathologic lymph node, suggesting a malignant process, therefore we decided surgical exploration (Fig. 1). A solid, malignantly appearing lesion was identified in the body and tail of the pancreas, infiltrating the splenic hilum and transverse colon. A pylorus-preserving total pancreatectomy with splenectomy and extended right hemicolectomy was performed with an uneventful postoperative recovery (Fig. 2).
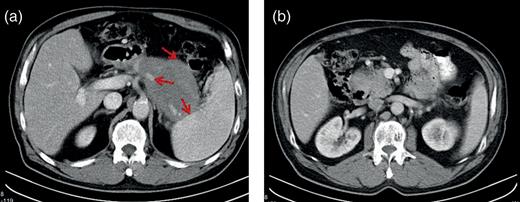
Preoperative CT scans. (a) The pancreatic mass in the tale of the pancreas, the arrows shows the relationship to the colon, to the spleen and to the splenic artery and (b) the pancreatic mass in the head of the pancreas.

Macroscopic specimen (two separate pancreatic mass in the head and in the tale of the pancreas + duodenum + colon + spleen).
On histological examination, both lesions contained elongated spindle cells, infiltration of plasma cells, lymphocytes, histiocytes and eosinophilic granulocytes. There was no evidence of malignancy. Large number of plasma cells were IgG positive, and 40% of the cells were IgG4 positive (Fig. 3).
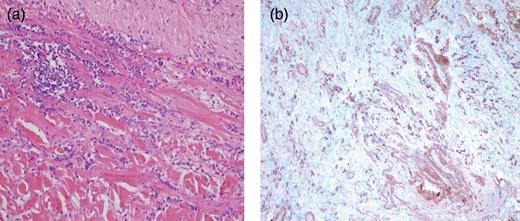
Histopathologic examination of the pancreatic mass: (a) HE and (b) IgG4 immunohistochemistry.
Laboratory tests proved an elevated IgG4 level (2.4 g/l).
DISCUSSION
About 20% of AIP is still diagnosed after surgical resection. The question arises whether it is possible to reduce the number of unnecessary operations, since AIP can be treated with steroids [5–7].
Diagnostic work up based on the International Consensus Diagnostic Criteria [1].
Endoscopic retrograde cholangiopancreatography (ERCP) images can be so characteristic, which combined with any other positive test result can confirm the diagnosis of AIP. Our patient had no jaundice, so the indication for preoperative ERCP was not self-evident—perhaps this test could have brought us closer to the diagnosis.
CT, MRI or Magnetic Resonance Cholangiopanreatography (MRCP) can also show typical signs (sausage-like broadening, infiltration of adipose tissue, ring-like delayed contrast enhancement and altering density distribution), but alone none of the tests is sufficient to verify the diagnosis.
Transabdominal or endoscopic ultrasound-guided pancreatic Fine Needle Aspiration Biopsy (FNAB) is a valuable method detecting pancreatic cancer. However, a negative cytological finding does not exclude pancreatic cancer. Whenever AIP is suspected, EUS–FNAB or core biopsy is recommended, and alone the positivity of this test is sufficient for making the diagnosis. Demonstrating v-Ki-ras2 Kirsten rat sarcoma viral oncogene homolog (KRAS) mutations from the FNAB sample further helps to distinguish AIP for malignant pancreatic disease, since KRAS mutation is found in 90% of patients with pancreatic cancer, but never in AIP [8, 9].
The serum IgG4 level can be elevated up to 70–90% in AIP type 1; however, 10% of pancreatic cancers can present with an increased IgG4. A 2-fold increase of IgG4 concentration could be the watershed value.
Elevated CA 19-9 level is typical for ductal pancreas adenocarcinoma; however, a slight increase of CA 19-9 levels can be observed in 20% of AIP patients as well, but rarely elevated above 200 U/ml [7, 10].
AIP responds well to steroid therapy. If this disease is suspected, a so-called ‘steroid trial’ might be used. However, patients with pancreatic cancer can also experience a lessening of their complaints; therefore, this ‘trial’ could be used only by patients with tumor-negative core biopsies, in specialized centers when other AIP-specific criteria are present [8].
Focal lesions of the pancreas should always be considered as malignant, unless other disease cannot be unequivocally verified. On the other hand, retrospectively analyzing this case, we came to the conclusion that even in the case of a pancreatic lesion described by the imaging studies as clearly malignant, a possibility of a rare disease such as AIP should be taken into consideration. This could change the treatment dramatically.
AUTHORS’ CONTRIBUTIONS
KD proposed the study. KD and DT performed research and wrote the first draft. FS, AT collected the data. All authors contributed to the design and interpretation of the study and to further drafts. AB is the guarantor. Ethical approval is not required for this study.
Conflict of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.



