-
PDF
- Split View
-
Views
-
Cite
Cite
Oliver Varban, Ali Tavakkoli, Multiple simultaneous small bowel intussusceptions in an adult, Journal of Surgical Case Reports, Volume 2012, Issue 11, November 2012, rjs011, https://doi.org/10.1093/jscr/rjs011
Close - Share Icon Share
Abstract
Intestinal intussusception is a rare cause of bowel obstruction in adults and can be associated with a pathologic lead point. We report a case of multiple simultaneous small bowel intussusceptions in a 41-year-old female who presented with a 3-week history of intermittent, crampy epigastric abdominal pain, nausea and diarrhea. Computed tomography imaging demonstrated two areas of intussusception. The patient underwent exploratory laparoscopy, and six separate regions of intussusception were discovered.
INTRODUCTION
Adult intussusception (AI) is a rare cause of bowel obstruction and is often associated with a pathologic lead point located in a single region of bowel. The mechanism of intussusception is not fully understood, but it is believed to result from a lesion in the bowel wall that alters the peristaltic pattern of the bowel causing invagination. In cases where no lead point is identified, intussusception may be due to submucosal bowel edema, fibrous adhesions or dysrhythmic contractions [1].
The management of intussusception in adults differs from that of children, where the diagnosis is more common and treatment is based primarily on radiological reduction. Surgical resection is recommended in cases of AI because it has been associated with a lead point in up to 95% of cases [1–3]. However, given the abundant utilization of abdominal imaging, AI is also diagnosed incidentally in asymptomatic patients, in which no clinical sequelae occur and surgery is not indicated [4]. This results in a diagnostic and therapeutic dilemma, particularly in a patient with multiple simultaneous regions of small bowel intussusception.
CASE REPORT
A 41-year-old female presented with 3 weeks of intermittent crampy epigastric abdominal pain, nausea and diarrhea. She was able to tolerate a liquid diet but not solids. She had one episode of vomiting and lost 6 lbs over the course of 3 weeks. Her vital signs, physical examination and laboratory studies were unremarkable. She did not have a history of prior abdominal surgery or malignancy. A CT scan demonstrated two areas of small bowel intussusception (Fig. 1A and B), without evidence of bowel obstruction or mass. The patient underwent exploratory laparoscopy using a 5 mm 30° camera and two 5 mm working ports. Six separate regions of intussusception within the small bowel were discovered between 55 and 130 cm from the ligament of Treitz. All areas of intussusception were short and witnessed to undergo spontaneously reduction (Fig. 2A and B), except for one (Fig. 3), which was resected through a mini-laparotomy. There was no obvious evidence of masses, adhesions or serosal abnormalities along the small bowel. There were prominent lymph nodes noted in the small bowel mesentery (Fig. 4). The postoperative course was uneventful and she was discharged 4 days after her operation. She had resolution of symptoms and had no recurrence after 3 years of follow-up. Pathologic examination of the small bowel demonstrated no evidence of malignancy, lead point, pathologic changes or sprue. Likewise, there was no evidence of acid-fast organisms, fungal or helminth parts identified. The enlarged mesenteric lymph nodes demonstrated reactive follicular hyperplasia and multifocal non-necrotizing lipogranulomas.
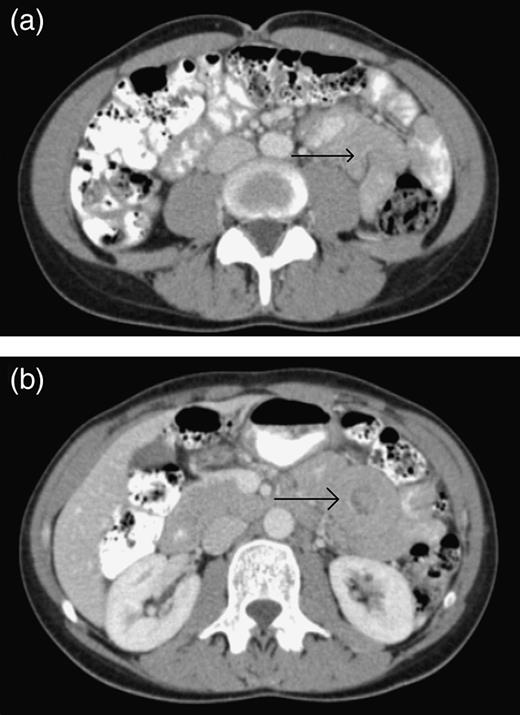
(a) The CT scan of the abdomen demonstrating an area of small bowel intussusception (arrow) resulting in a mushroom sign. (b) The CT scan of the abdomen demonstrating an area of small bowel intussusception (arrow) resulting in a target sign.
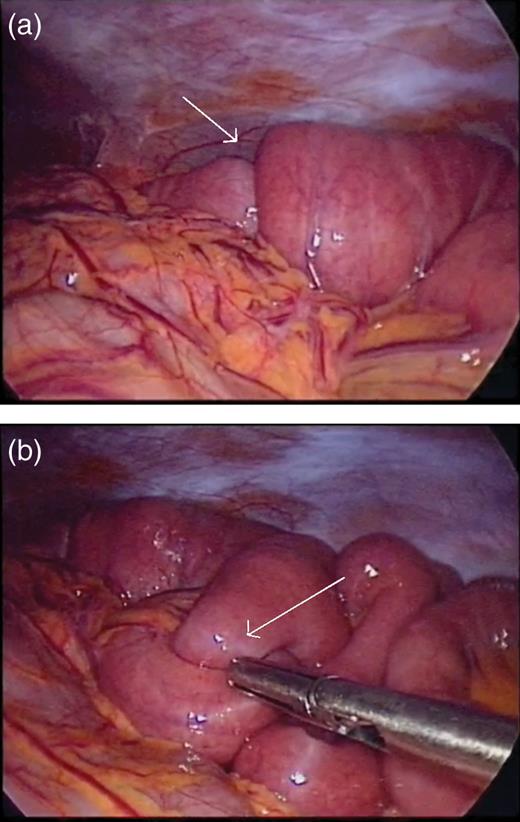
(a) Short segment of small bowel intussusception (arrow) that reduced spontaneously during laparoscopy. (b) A separate segment of small bowel intermittently intussuscepting and reducing (arrow) during laparoscopy.
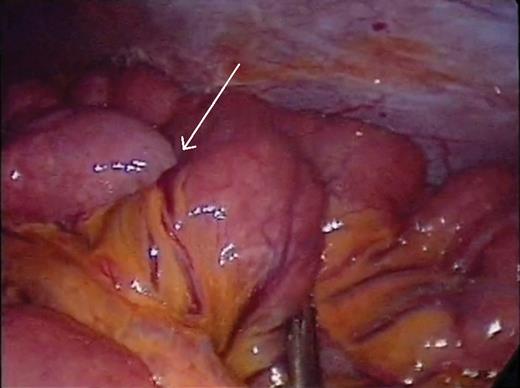
Small bowel intussusception (arrow) that did not reduce spontaneously.
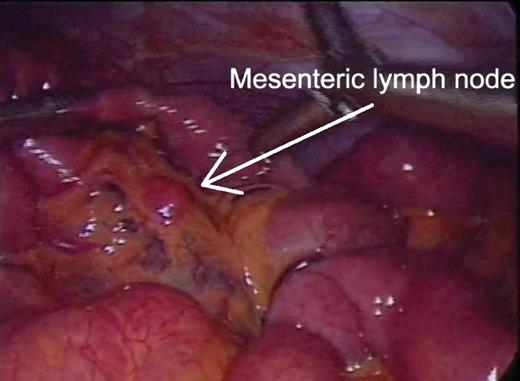
Prominent mesenteric lymph nodes (arrow) discovered during laparoscopy.
DISCUSSION
Management of symptomatic AI is often considered surgical because of the likelihood of identifying a lead point [1–3]. However, the growing use of CT scans has led to increased detection of transient intussusceptions with no underlying disease [4–5]. This is the first reported case in which multiple transient simultaneous small bowel intussusceptions have been identified intraoperatively.
Short segments of small bowel intussusception appear to reduce spontaneously and do not necessarily require excision. Segments with persistent intussusception should be excised as they may contribute to symptoms of obstruction or may harbor a malignancy. Laparoscopy offers a minimally invasive approach to managing symptomatic AI as well as in cases where the diagnosis is not clear.



