-
PDF
- Split View
-
Views
-
Cite
Cite
Anjan Kumar Dhua, Badamutlang Dympep, Amita Sen, Obstructive jaundice due to pancreatic pseudocyst in a pediatric patient, Journal of Surgical Case Reports, Volume 2012, Issue 11, November 2012, rjs009, https://doi.org/10.1093/jscr/rjs009
Close - Share Icon Share
Abstract
Obstructive jaundice solely due to pancreatic pseudocyst is rare in pediatric patients. Successful management of a case by internal drainage is being described here. The role of intra-operative cholangiogram is being highlighted for deciding whether a simple drainage procedure would be required instead of a hepatico-jejunostomy.
INTRODUCTION
A pancreatic pseudocyst can theoretically cause obstructive jaundice especially those arising at the head of the pancreas. Since majority of the pseudocysts arise from the body and tail, they rarely produce obstructive jaundice [1]. We present a previously asymptomatic boy with a mass in the abdomen and obstructive jaundice found to be having a pseudocyst of pancreas during operation. The finer aspects of management of such a case and the pertinent literature are discussed.
CASE REPORT
An 8-year-old boy presented to our hospital with jaundice and intermittent pain in the abdomen since last 1 year after a trivial blunt abdominal trauma sustained while at play. Jaundice was insidious and was gradually progressive and was associated with upper central abdominal pain which was intermittent. Pain was not radiating and of no specific character. There was no history of fever, bowel or urinary complaints. Past history was unremarkable. The patient was icteric and abdominal examination revealed a solitary mass in the upper mid-abdomen which was oval in shape and measuring 15 cm vertically and 10 cm horizontally. The upper margin was imperceptible from the inferior liver edge. It was not tender and not mobile. The liver edge was palpable 3 cm below the right costal margin. A clinical diagnosis of choledochal cyst was made and further investigated. Hemogram was within the normal limits. Liver function tests showed: total bilirubin was 2.8 mg/dl (direct 2.4 mg/dl), normal enzymes and raised alkaline phosphate (3881 U/l). Sonography was suggestive of choledochal cyst with hepatomegaly. Magnetic Resonance Cholangiopancreatography (MRCP) gave a picture of a type 1 choledochal cyst (Fig. 1a).
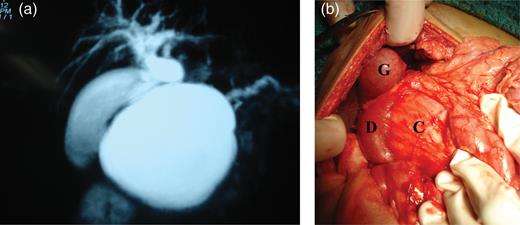
(a) MRCP with 2D-reconstruction demonstrating features indicating a type 1 choledochal cyst, (b) intra-operative showing gallbladder (G), duodenum (D) stretched and compressed with widened C loop of duodenum and the pseudocyst (C) within.
The patient was operated and the intra-operative findings (Fig. 1b) were of a large pseudocyst of pancreas arising predominantly from the head and body of the pancreas. The ‘C loop’ of the duodenum was splayed and stomach was pushed up anteriorly. Gall bladder and the portal anatomy were normal. The liver was enlarged and surface had fine nodules. There was no sign of active pancreatitis. An intra-operative cholecystogram was performed that showed unequivocal obstruction of the terminal common bile duct (CBD).
A cysto-gastrostomy was performed along with a liver biopsy. Following decompression, the anatomy of structures around the ‘C Loop’ of duodenum normalized. A repeat cholecysto-cholangiogram could not be repeated due to technical reasons; hence, a tube cholecystostomy was performed to drain the obstructed biliary system and to have an access for postoperative cholecysto-cholangiogram. The post-operative course was uneventful. Bilirubin dropped to 1.9 mg/dl (direct 1.1 mg/dl). A repeat contrast study was arranged on the 10th post-operative day to demonstrate free passage of contrast across the biliary tree into the duodenum (Fig. 2a). Histopathology of the disk of tissue from the common wall between stomach and the pseudocyst showed features of pancreatic pseudocyst. The liver biopsy (Fig. 2b) showed features of chronic extra-hepatic biliary obstruction. After 3 months of follow-up, the patient is asymptomatic and is anicteric. Work up for etiology of pancreatic pseudocyst was done and no specific cause could be ascertained, hence attributed to trauma. However, an endoscopic retrograde cholangiopancreatography (ERCP) is also being planned to rule out pancreas divisum as a cause of pancreatitis.
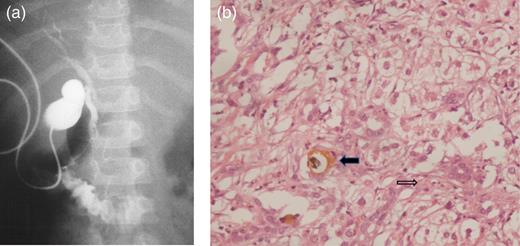
(a) Post-operative cholecysto-cholangiogram demonstrating passage of contrast across the biliary tree into the duodenum. (b) Bile duct proliferation (thin arrow) and bile plug (bold arrow) (H&E, ×20).
DISCUSSION
Pancreatic pseudocyst as the sole cause of external compression and jaundice is rare [2, 3]. The usual rare setting is that of a patient with alcoholic chronic pancreatitis and jaundice. This is usually due to hepatocellular damage or in addition to compression and narrowing of the terminal CBD due to fibrosis, each contributing to produce jaundice.
In order to provide clarity to the patho-physiology of pseudocysts causing jaundice, Sidel et al. [1] proposed that four criteria must be met in order to prove that pseudocyst is the only culprit. They are: (i) presence of biliary obstruction, (ii) demonstration that the CBD is compressed by the pseudocyst, (iii) relief of biliary obstruction by drainage of the pseudocyst, (iv) complete disappearance of jaundice in the postoperative period. Our patient fulfilled each criterion and thus it was concluded that jaundice in our patient was solely because of the compression effect by the pseudocyst.
The management is not straightforward as is the diagnosis. One could argue that a hepatico-jejunostomy must have been done at the outset, as Warshaw et al. [2] rightly emphasized that bilio-enteric bypass must be strongly considered when dealing with this kind of a disease process. Mehta et al. [4] also reported three patients with jaundice due to pseudocysts and emphasized the importance of the bypass procedure because a simple drainage procedure did not relieve the obstructive process in their patients. In our case, the intra-operative cholecysto-cholangiogram made us to believe that the compression was really due to the pseudocyst. The disposition of structures normalized after decompressing the cyst, thus the idea of deferring a choledocho-jejunostomy. This decision should have been tested intra-operatively by a repeat cholecysto-cholangiogram, unfortunately it could not be done due to technical reasons and hence an access for performing a dye study was left in the form of cholecystostomy. This channel also provided a rapid decompression of the entire hepato-biliary tree in the post-operative period and subsequent decline in the bilirubin levels. The favorable postoperative dye study results substantiated our intra-operative decision. Subsequent work up did not reveal any recurrent cause for pancreatitis; hence, this also supports our conservative approach.
Observations similar to ours have been reported by Cho et al. [5] and Gonzalez et al. [6]. McCollum et al. [7] and Skellenger et al. [3] showed that decompression in the form of cysto-duodenostomy was successful in treating jaundice. Thus, in the literature both forms of management have been described; however, emphasis must be put on the importance of intra-operative cholangiogram for determining the actual operative technique that is suitable for a particular patient.
After reviewing the English literature, it is our belief that this case is the first pediatric case of obstructive jaundice occurring solely because of a pancreatic pseudocyst and treated successfully with internal drainage alone.
This case also illustrates the fact that MRCP may not bring out the true anatomical picture especially in a child [8]. In hindsight, an ERCP probably would have settled the issue in the preoperative period itself, but ERCP is generally not resorted because of the invasive nature of the examination and exposure to radiation. ERCP is however warranted now in follow-up to rule out pancreas divisum as a cause of pancreatitis and also to countercheck the patency of CBD despite the patient being anicteric.
In a pediatric patient with a triad of pain, jaundice and a mass, one must also keep pancreatic pseudocyst as a differential. An intra-operative cholangiogram is indispensable for accurate decision-making. If strict criteria are met, the simple drainage procedure can be therapeutic for this rare complication.



