-
PDF
- Split View
-
Views
-
Cite
Cite
A Guner, S Karyagar, O Ozkan, C Kece, E Reis, Parathyroid cyst: the forgotten diagnosis of a neck mass, Journal of Surgical Case Reports, Volume 2011, Issue 8, August 2011, Page 4, https://doi.org/10.1093/jscr/2011.8.4
Close - Share Icon Share
Abstract
The differential diagnosis of cystic cervical masses includes cystic thyroid disease or some embryological diseases. Parathyroid cyst is one of the less common causes of the cervical masses. The Swedish anatomist Sandstrom reported the first description of parathyroid cyst in 1880. Up to date, only about 300 cases have been reported in the world literature. They may be functional or nonfunctional, depending on the presence or absence of the hyperparathyroidism and treatment options vary for both presentations. Particularly, nonfunctional cysts are often considered as thyroid cysts. Diagnosis is best made by monitoring serum calcium levels and sending cyst fluid for parathormone analysis.
We herein report a patient diagnosed with a parathyroid cyst who had received the diagnosis of goitre at other institute; including a review of the literature.
INTRODUCTION
The differential diagnosis of cystic cervical masses includes thyroid cyst, thymic cyst, thyroglossal duct cyst, branchial cleft cyst, bronchogenic cyst, lymphangioma and parathyroid cyst (PC) (1). PC is one of the less common causes of the cervical masses. The Swedish anatomist Sandstrom reported the first description of PC in 1880. Since then, approximately 300 cases have been reported in the world literature (2). They may be functional or nonfunctional, depending on the presence or absence of the hyperparathyroidism and treatment options vary for both presentations.
We herein report a patient diagnosed as PC and treated conservatively, while reviewing of the literature.
CASE REPORT
A 56-year-old woman presented with a left-sided cervical lump with three months history. She had been received the diagnosis of goitre at other institute. No dyspnea, swallowing disturbance or voice changes were recorded. At the physical examination, a soft, roundish, painless mass was palpable on the left side of thyroid. Ultrasound of the neck revealed a cystic mass in the left lower pole of the thyroid 2×1 cm in size and the radiologist suspected the diagnosis of thyroid nodule or parathyroid mass (Figure 1).

Ultrasonographic view of the neck revealed a cystic mass in the left pole of the thyroid
Thyroid function tests including triiodothyronine, thyroxin and thyroid-stimulating hormone were normal. Intact parathyroid hormone (PTH) level was 34 pg/mL (normal, 15-65 pg/mL), serum calcium level was 9.8 mg/dL (normal, 8.4-10.2 mg/dL) and phosphorous was 4.3 mg/dL (normal, 2.6-4.5 mg/dL). Sestamibi scintigraphy was performed and it did not show any focal uptake (figure-2).
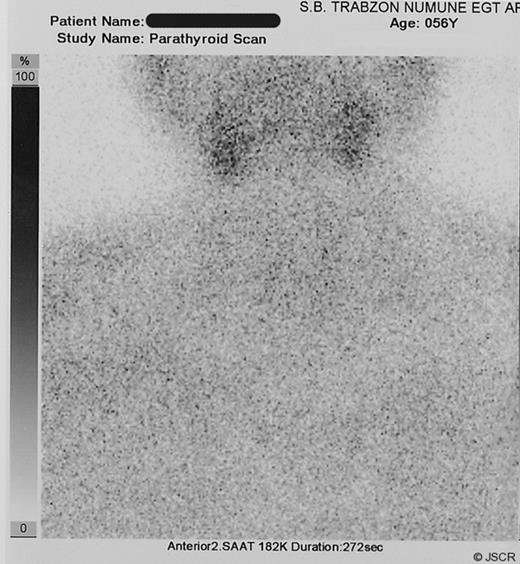
Sestamibi scintigraphy shows no focal uptake for parathyroid disease
Fine needle aspiration (FNA) was performed under ultrasound guidance; 5 ml clear colorless fluid was removed and complete collapse of cyst was obtained. These findings led us to suspect a parathyroid cyst. Cytological examination of the fluid was acellular, however, intact PTH level of the fluid was 261 pg/mL. Because of no evidence of hyperparathyroidism, conservative follow-up was decided. After six months of initial aspiration, there was no recurrence either physical examination or ultrasound evaluation.
DISCUSSION
PC is rare clinical entity and about 300 cases have been reported in the literature up to this time. In 1880, Sandstrom reported first description of PC and Goris reported the first successful resection of a cervical PC in 1905 (1).
Several theories have been suggested for the development of PC including persistent embryologic remnant of pharyngeal pouches, an accumulation of secretions, enlargement of pre-existing microcysts and cystic degeneration of parathyroid adenoma (3). Ippolito described the compatibility between the embryologic remnant theory and 38 true PCs, in the one of the largest case series in the literature (4). Various combinations of different tissues as lymphoid, thymic, salivary, adipose, mesenchymal, were found in the cyst wall and these findings were suggestive of branchial origin. As compatible with this theory, all cysts had originated from inferior parathyroid gland as our presented case. Some PCs arise from a pre-existing adenoma or a hyperplastic gland, however these are not true cysts. They consist of cystic degeneration of pre-existing lesion, therefore, usually presenting with hyperparathyroidism.
Traditionally, PCs are classified as functional or nonfunctional, the former being associated with clinical hyperparathyroidism. Nonfunctional cysts are more common and the majority of patients, nearly 91%, have nonfunctioning cysts (5). Functional cysts, derived from parathyroid adenomas that underwent central necrosis and degeneration and account for 1% of all cases of hyperparathyroidism (6). Symptoms of nonfunctional cysts depend on the compression of neighboring structures; therefore they are usually asymptomatic and found incidentally. Neck swelling may be associated with dysphagia, odynophagia and paralysis of the recurrent laryngeal nerve (7). Rarely, cysts occur in the mediastinum and patients are admitted with respiratory symptoms. In the Ippolito’s case series, most common presentation was an asymptomatic cystic lesion that was detected incidentally during cervicotomy to treat a thyroid nodule. The location of the cysts differs between the two groups. For the nonfunctioning cysts, the inferior glands are most commonly involved, with the left-sided predominance. However, functional cysts have been located anywhere from the angle of the mandible to the mediastinum. In contrast to our knowledge, McCoy and colleagues reported that functional PCs are much more common than nonfunctional PCs and they have an equal affinity for superior and inferior glands (8). Our presented patient did not have any considerable symptom. She only detected a cervical swelling 3 months ago by herself. There were no laboratory abnormalities and she was normocalcemic.
Ultrasonography, computerized tomography or magnetic resonance imaging can help to distinguish whether the mass is solid or cystic, however differentiating of thyroid tissue from parathyroid tissue are often experience dependence (6). FNA is the main diagnostic tool for cystic lesions. When intracystic fluid is water-clear and colorless, it is very suggestive of a parathyroid origin (9). Evaluation of the intracystic level of PTH is more important than the appearance of the fluid. PTH levels are increased in all PCs independently of whether they are functioning or nonfunctioning. Both the carboxy-terminal PTH (inactive form of PTH) and intact PTH (bioactive form) levels may be elevated. However, it is recommended that carboxy-terminal PTH rather than the intact PTH is requested on fluid obtained from a suspected parathyroid mass (10). Because of the correlation between the number of oxyphil cells and abnormal parathyroid tissue visualization in sestamibi scintigraphy, it rarely yields positive results for PCs. For the presented case, after suspicion for the PC, when a mass was detected on the ultrasonographic evaluation, FNA was performed; physical characteristics and PTH level of the fluid confirmed the diagnosis of PC. Cytologic evaluation of the fluid and scintigraphy were insufficient.
Treatment options for PC include aspiration, sclerosing therapy and surgical excision. FNA with cystic fluid assay for PTH levels represents the approach of choice for both diagnosis and the initial treatment. This approach is more effective for nonfunctioning cysts, particularly. Sclerosing therapy can be used as an alternative therapy by ethanol or tetracycline; however, it may be associated with many complications as neck pain, neurotoxicity and recurrent nerve palsy. If repeated aspiration is unsuccessful, cyst is symptomatic or a functional cyst is present, surgical resection is the best option (3,4,7). However, McCoy recommends the surgical therapy for all PCs regardless of functional status because of the low morbidity of surgery. For presented case, we have preferred the conservative approach by aspiration, follow-up and re-aspiration when necessary. After the definitive diagnosis, this approach is the best option for asymptomatic, nonfunctional cyst regardless of its size.
In conclusion, PCs are rare lesion and often considered as thyroid cysts. Diagnosis is best made by monitoring serum calcium levels and sending cyst fluid for PTH analysis. Therefore, PCs must be included and be remembered within the differential diagnosis of all neck swelling.



