-
PDF
- Split View
-
Views
-
Cite
Cite
S Ray, K Das, Gossypiboma presented as abdominal lump seven years after open cholecystectomy, Journal of Surgical Case Reports, Volume 2011, Issue 8, August 2011, Page 2, https://doi.org/10.1093/jscr/2011.8.2
Close - Share Icon Share
Abstract
Gossypiboma is very rare in clinical practice. Despite its clinical importance, it carries some medico legal implications. We report a case of gossypiboma in a 54 years old female who presented with pain and a slowly growing lump in the abdomen 7 years after open cholecystectomy. Computed tomography (CT) scan of the abdomen showed a mass with enhanced internal septae and a radio-opaque marker within it, raising the suspicion of a foreign body. She underwent excision of the mass along with a segment of densely adherent transverse colon. Post-operative recovery was uneventful and the patient was well at 19-month follow up.
INTRODUCTION
The term Gossypiboma, derived from the Latin word “gossypium” (cotton) and the Swahilli “Boma” (place of concealment) (1) denotes retained surgical sponge. The condition may manifest as an exudative inflammatory reaction with formation of abscess or aseptic fibrotic reaction with formation of a mass (2). The patient may present early with features of sepsis or may remain asymptomatic or may present with non-specific symptoms months or years after the operation. Although early recognition of this problem will ensure institution of appropriate treatment, every measure should be taken to prevent this complication. Herein, we report a case of gossypiboma presented as an abdominal lump 7 years after open cholecystectomy.
CASE REPORT
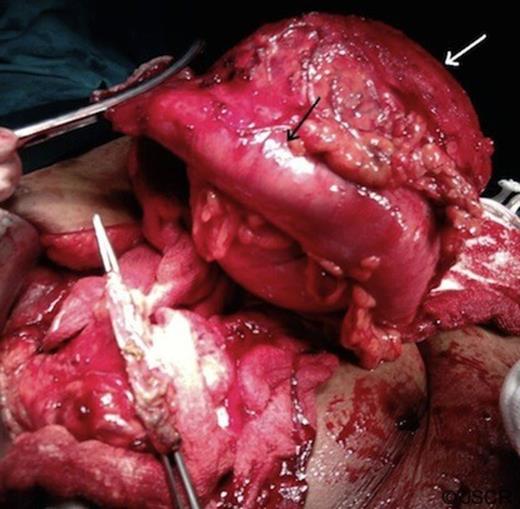
A 54-year-old woman presented with a 2-years history of dull aching pain in the upper abdomen and 1 year history of an abdominal swelling. She underwent open cholecystectomy 7 years back. She developed fever and purulent discharge from the wound in the immediate postoperative period which was treated conservatively. On examination a large non-tender mass with restricted side to side mobility was found in the right hypochondrium extending up-to the right lumber region. Blood investigations revealed hemoglobin of 8.5Gm/dl, leukocyte count of 9600/mm3, serum bilirubin of 2.9 mg/dl and alkaline phosphatase of 507 U/L. The plain abdominal radiography did not show any sign of a radio-opaque marker in the abdomen. However, contrast enhanced abdominal computerized tomography revealed a 15×12x10 cm round well-defined soft-tissue mass with multiple septae. The wall of the lesion and septae showed mild contrast enhancement (Figure-1).

CT scan abdomen (both oral and intravenous contrast) showed a mass in right upper quadrant with displacement of gut loops towards the left. The mass showed contrast enhanced internal septa (white arrow)
A radio-opaque material was seen in the lesion raising the suspicion of a foreign body. Common bile duct was dilated and contained a stone which was removed endoscopically. At exploration, a large globular lesion was found which was densely adhered to the adjacent structures (anterior abdominal wall, omentum, transverse colon, and antrum of the stomach). En-bloc resection of the mass along with the adhered transverse colon was done (Figure-2). Cut section of the mass showed a large surgical sponge and a foreign body within it (Figure-3).The patient had an uneventful recovery and she was well at 19-month follow-up.
Operative photograph showing a large mass (white arrow) with adherent transverse colon (black arrow).
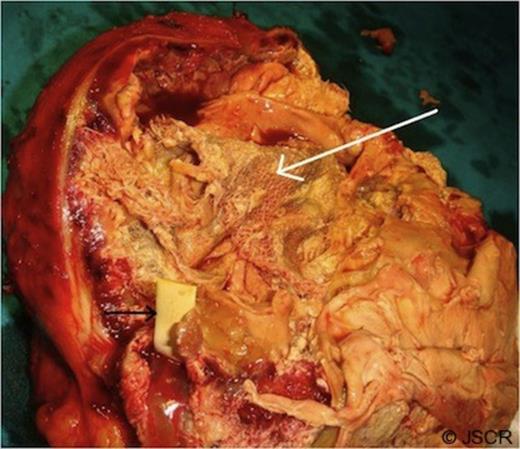
Cut section of the mass showing a large sponge (white arrow) and a radio-opaque marker (black arrow) within it.
DISCUSSION
Gossypiboma or a mass of cotton that is retained in the body following surgery is rarely seen in daily clinical practice. Although the real incidence is unknown, it has been reported as 1 in 100 to 3000 for all surgical interventions and 1 in 1000 to 1500 for intraabdominal operations (3,4)
The clinical presentation of gossypiboma varies and depends on the location of the sponge and the type of reaction. The sponges are inert in human tissue and do not undergo decomposition. There are 2 types of foreign body reaction in pathology: an exudates reaction leading to abscess formation or chronic internal or external fistula formation, and an aseptic fibrinous reaction resulting in adhesion, encapsulation, and eventual formation of granuloma of various size. The latter usually presents much later than exudates reaction sequelae. They usually remain asymptomatic or present with pseudotumor syndrome, as in our case.
Because, the symptoms of gossypiboma are usually nonspecific and may appear years after surgery, the diagnosis of gossypiboma usually comes from imaging studies and a high index of suspicion. The most impressive imaging finding of gossypiboma is the curved or banded radio-opaque lines on plain radiograph.
The ultrasound feature is usually a well-defined mass containing wavy internal echogenic focus with a hypoechoic rim and a strong posterior shadow. However, this is often misinterpreted due to its clinical rarity (5). On CT scan, a gossypiboma may manifest as a cystic lesion with internal spongiform appearance with mottled shadows as bubbles, hyperdense capsule, concentric layering, or mottled mural calcifications (6). When no radio-opaque marker is seen on X-ray or CT, the characteristic internal structure of the gauze granuloma is best visualized on magnetic resonance imaging. It may appear as a low-signal-intensity lesion on T2-weighted images with wavy, striped or spotted appearance (7).
Once gossypiboma is diagnosed, it should be removed. Surgery had been the mainstay of therapy for many years. However, some reports recommending alternative methods have recently appeared in the literature. Nosher and Siegel (8) described six patients in whom percutaneous extraction was successfully performed for removal of foreign bodies.
Besides diagnostic and therapeutic difficulties, gossypiboma carries some medico-legal implications. The presence of a foreign body inside the patient can be easily proved and the patient may litigate the responsible surgeon because this is an avoidable problem. Moreover, gossypiboma may be misdiagnosed as a malignant tumor and lead to unnecessary invasive diagnostic procedures or extensive extirpative surgery (as in our case) which may result in further complications (9). Prevention is the best treatment as in many other medical problems. Avoidance of leaving foreign bodies inside the patients could be possible by implementation of three measures: meticulous count of all surgical materials, thorough exploration of the surgical site at the conclusion of the procedures and routine use of surgical textile materials impregnated with a radio-opaque marker.
Gawande et al (3) published an article about risk factors of retained foreign bodies (RFBs). Of the 8 risk factors, the authors identified [emergency operation, unexpected change in operation, more than one surgical team involved, change in nursing staff during procedure, body mass index (BMI), volume of blood loss, female sex, and surgical counts] only 3 were found to be statistically significant by multivariate logistic regression. The 3 significant risk factors were emergency surgery, unplanned change in the operation, and BMI. The counting of sponges and instruments was not a significant predictor in the multivariate model. Although all 3 factors were significant, the 9-fold increase in risk associated with emergency surgery was impressive. In addition, in 88% of the cases where there was a RFB and counts were performed, the counts were falsely called correct. The authors recommended “radiographic screening” at the end of high risk cases as a possible adjunct to improve detection of RFB.
Although human errors cannot be completely avoided, continuous medical training and strict adherence to rules of the operation room should reduce the incidence of gossypiboma to a minimum.



