-
PDF
- Split View
-
Views
-
Cite
Cite
J Klcova, S Mathankumara, P Morar, A Belloso, A rare case of necrotising epiglottitis, Journal of Surgical Case Reports, Volume 2011, Issue 2, February 2011, Page 5, https://doi.org/10.1093/jscr/2011.2.5
Close - Share Icon Share
Abstract
We report a case of an acute necrotizing supraglottitis in a healthy patient. Only seven cases of necrotizing epiglottitis/supraglottitis have been reported in medical literature; all in immunocompromised patients. The features and characteristics of necrotizing epiglottitis are discussed with review of all previously reported cases.
INTRODUCTION
We report a case of an acute necrotizing supraglottitis in a healthy patient. Only seven cases of necrotizing epiglottitis/supraglottitis have been reported in medical literature; all in immunocompromised patients. The features and characteristics of necrotizing epiglottitis are discussed with review of all previously reported cases.
CASE REPORT
A 65-year-old male presented in the Emergency department complaining of a two day history of dysphagia, dysphonia, neck pain and a sore throat; that rapidly evolved to stridor and dyspnoea. There was no history of trauma.
His past medical history included vascular sarcoma treated with above knee amputation and chemotherapy 10 years ago, non insulin dependent diabetes mellitus (NIDDM) as a result of chemotherapy and hypertension. He is an ex smoker for 20years ago.
Initial clinical evaluation revealed a biphasic stridor with laboured breathing. The respiratory rate was 21/min with 100% SpO2 on15 l/min O2. He was plethoric with tachycardia (116 bpm), hypertensive (136/92 mmHg) and pyretic (38oC). Chest ausculation was normal. Neck palpation revealed 3 x 2 cm midline suprahyoid diffuse swelling with associated right sided level II lymph nodes. Soft palate and the oropharynx were inflamed. Oral cavity was normal with good dental hygiene.
The patient was intubated in the theatre and direct laryngoscopy demonstrated an oedematous supraglottis with redundant patchy necrosis occluding the glottis. Subsequently he was transferred to Intensive Care Unit and treated conservatively with dexamethasone and antibiotics (Table 1). There was no improvement in the patient clinically or by laboratory parameters. Daily nasal endoscopy findings showed progressive supraglottic soft tissue oedema, worsening necrosis, pooling of saliva and diminishing air leak around the orotracheal tube.
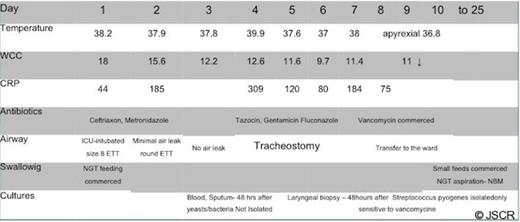
The contrast CT scan of the neck was performed on day 4 (Fig 1.), showing soft tissue oedema around the orotracheal tube, oropharynx and laryngopharynx extending from the posterior aspect of the hyoid bone down to the level of the thyroid cartilage. There was no fluid or pus collection.
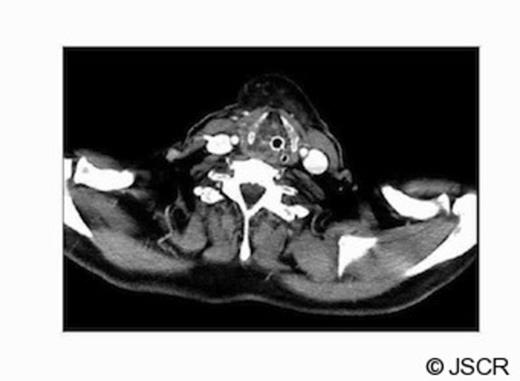
The contrast CT scan of the neck performed on day 4; showing soft tissue oedema around the orotracheal tube, oropharynx and laryngopharynx
On the same day, the patient was re-evaluated under general anaesthesia. Direct laryngoscopy revealed an extensive oedematous supraglottis with severe necrosis involving the laryngeal inlet, base of the tongue and right tonsillar bed. Incision of the soft tissue drained foul smelling fluid with minimal bleeding during biopsy. Surgical debridement was not possible without compromising the integrity of the larynx due to extensive necrosis. Subsequently a tracheotomy was performed with a limited exploration of the neck, showing only inflamed soft tissues in the anterior compartment. There was no evidence of necrosis or collection of pus in the neck spaces.
After the operation, the diagnosis was revised to isolated necrotizing fasciitis of the larynx. The necrosis of the larynx was closely monitored. A combination of empirical antibiotic therapy was prescribed under guidance of microbiologist (Table 1). The antibiotic regimen made significant improvements in the laryngeal oedema (Fig 2), resolution of necrosis and inflammation of the laryngopharynx.

Histology of the laryngeal tissue reported scanty viable tissue overgrown with bacteria and there was no evidence of neoplasm or fungal infection. The aetiology of this extensive necrosis was not apparent on histology.
Microbiology cultures isolated alpha haemolytic streptococcus pyogenes (GAS), characteristic of necrotising fasciitis. GAS was resistant Cefotaxime, Penicillin and Tetracyclin and sensitive to Vacomycin (Table 1). No yeast or fungi were isolated therefore antifungal treatment was stopped. The blood cultures were persistently negative.
On discharge (25th day of hospital stay), there was no dysphagia, dysphonia or dyspnoea. The necrosis of the larynx was fully resolved and the laryngeal skeleton was intact. Mucosal regeneration was complete and vocal cords were normal.
DISCUSSION
Acute necrotizing supraglottitis is a rare airway emergency. It is a potentially fatal infection of the supraglottis and adjacent structures (1).
There are only seven cases of necrotizing supraglottitis reported in medical literature. The first case was reported in 1983 as an isolated necrosis of the epiglottis in a 21 year old female with lymphoid leukaemia (2). All seven reported cases were immunodeficient patients. Five adults with various immunodeficiencies (3); and two paediatric patients suffering from infection induced haemophagocytic lymphohistiocytosis and an HIV positive infant (4).
Alpha haemolytic Streptococcus pyogenes is responsible for most of necrotising fasciitis in the head and neck region. Streptococcus pyogenes is a common commensal micro-organism in humans. It is estimated that between 5-15% of normal individuals harbour the bacterium, usually in the respiratory tract, without signs of disease(5). As normal flora, S. pyogenes can infect when defences are compromised or when the organisms are able to penetrate the constitutive defences. When the bacteria are introduced or transmitted to vulnerable tissues, a variety of suppurative infections can occur. Invasive toxigenic infections can result in necrotizing fasciitis, myositis and streptococcal toxic shock syndrome.
The clinical presentation of our patient’s laryngeal necrosis was aggressive and there was poor response to first line antibiotic treatment. The mouth, throat and sputum specimens did not isolate any specific organisms. The alpha haemolytic Streptococcus pyogenes was isolated from the laryngeal biopsy cultures; showing sensitivity only to Vancomycin.
Patient suffered from chemotherapy induced NIDDM with good glycaemic control, but he was healthy otherwise. There was no evidence of post chemotherapy induced oro-pharyngeal mucositis and granulocytopenia. Screening tests for HIV infection and other possible immunodeficiency diseases were normal. This case indicates the possibilities of supraglottic necrosis following local infection in healthy patients.
All previously reported cases in the literature resulted in post-necrosis partial or complete loss of larynx. In this case, the laryngeal necrosis was limited to the mucosa and there was no loss of laryngeal skeleton. There are a number of reasons why the presenting patient had a complete recovery with an intact larynx. Firstly, his normal immune status could confer more resistance to infection expansion. Secondly, the early identification of the necrosis and aggressive antibiotic regimen could limit the infection invasion and tissue destruction.



