-
PDF
- Split View
-
Views
-
Cite
Cite
PE Coyne, T Teemul, B Dent, D Henderson, R Crabbe, T Garud, Submucosal lipoma of the large intestine masquerading as a colonic malignancy, Journal of Surgical Case Reports, Volume 2011, Issue 2, February 2011, Page 4, https://doi.org/10.1093/jscr/2011.2.4
Close - Share Icon Share
Abstract
Lipomas of the alimentary tract are rare tumours that can mimic malignant lesions. They are often small and asymptomatic although larger tumours can present with intusussception or as abdominal masses. We present a case of a transverse colon submucosal lipoma masquerading as a colonic adenocarcinoma leading to resection.
A 74 year-old-man was referred urgently for assessment with altered bowel habits, and lower abdominal discomfort along with a positive Faecal-Occult-Blood sample. Colonoscopy demonstrated a large polypoidal lesion at the hepatic flexure with ulceration. Biopsies were inconclusive. A staging CT scan confirmed a 3.3 x 4.3 x 3.4cm Polyp with colonic wall thickening suspicious of malignancy. An extended right hemi-colectomy was performed. Histology showed a large submucosal lipoma with 12 reactive lymph nodes.
Colonic lipoma often present as incidental findings detected on either imaging or endoscopically whilst investigating other symptoms. Their appearances can mimic colonic malignancy and surgical resection may be required.
INTRODUCTION
Gastrointestinal lipomas are rare, mostly small and detected incidentally during endoscopic examination (1). These tumours are benign proliferations of mature fatty tissue arising in the submucosa and predominately arise in the large intestine (51-70%) preferentially on the right side. They make up 0.035-4.4% of all intestinal neoplasm’s (2). The majority of symptomatic lesions occur in adults in the sixth decade of life (2). Lipohypertrophy of the ileo-caecal valve is classified as a variant of normal (1).
The vast majority are asymptomatic but they can manifest due to intussusceptions, ulceration leading to haemorrhage or iron deficiency anaemia, intestinal obstruction or present as an abdominal mass. Most are compressible and submucosal although they can rarely develop in the serosa and appear as a fold or polyp. Larger lesions can become lobulated or pedunculated. They contain mature adipose tissue and usually have a thick capsule surrounding the tumour (2). Secondary cellular changes can include nuclear hypertrophy, hyperchromasia and pleomorphism, fat necrosis. These changes if extensive can mimic a liposarcoma; however, frank liposarcoma of the colon is extremely rare and requires the presence of lipoblasts (2). Endoscopically mechanical trauma can worsen ulceration and suggest a malignant process. Mucosal biopsies can be unhelpful and yield either intact mucosa, granulation/inflammatory changes or fat necrosis. When the tumour is sampled away from ulcerated areas mature adipocytes will be found.
Lipoma of the colon mimicking adenocarcinoma is rare but poses a difficult clinical dilemma. It can be difficult to separate the two and even endoscopic ultrasound can be non-diagnostic and adequate histology sampling may require a resection (3). Where a biopsy diagnosis has been made endoscopic resection or limited resection can be undertaken removing the need for major resectional surgery (3). Where this is not technically feasible a minimally invasive approach using either mini-laparotomy or laparoscopic resection has successfully been reported (4,5).
CASE REPORT
A 74 year old man with a background of Chronic Obstructive Airways Disease (COAD) was referred for urgent assessment by his general practioner with a 1 month history of lower abdominal pain and altered bowel habit. Faecal occult blood testing was positive. Abdominal and rectal examination was unremarkable and routine blood testing including carcinoembryonic antigen (CEA) was normal. He underwent urgent colonoscopy which was complete to the caecum. A large ulcerating polypoidal lesion was found at his hepatic flexure (Figure 1).
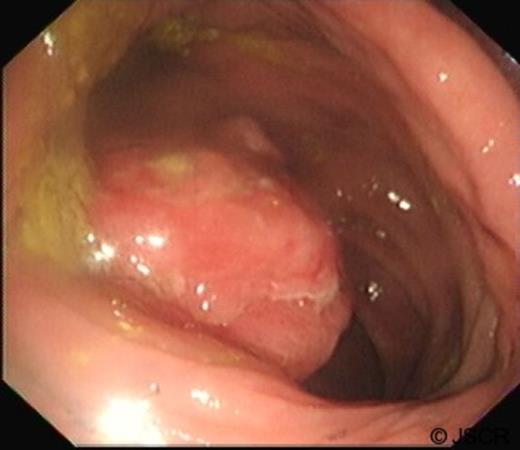
Colonoscopy demonstrating large pedunculated ulcerating lesion found at hepatic flexure
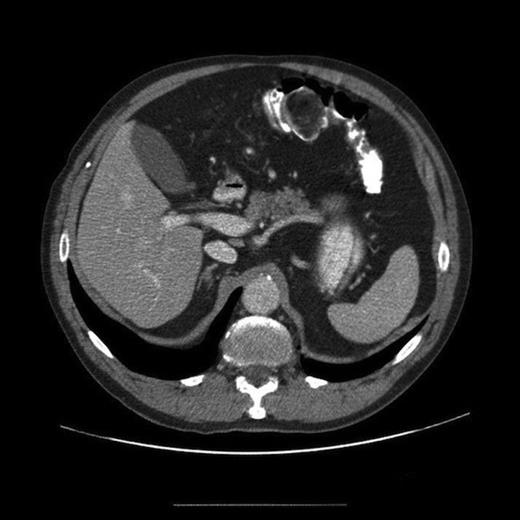
Histology from biopsies taken showed no evidence of neoplasia or dysplasia but was felt to most likely be unrepresentative of the endoscopic lesion. A staging CT scan of chest, abdomen and pelvis was arranged as part of pre-operative staging protocol and this demonstrated a large 3.3 x 4.3 x 3.4cm heterogeneous enhancing colonic polyp, which predominately enhanced with fatty attenuation (Figure 2). Proximal to the lesion was circumferential colonic wall thickening and surrounding fat stranding suspicious of colonic malignancy. A small node was seen in the vascular pedicle. No distant metastases were identified. There was concern about colonic malignancy and following discussion at a MDT meeting he was offered a surgical resection.
A laparoscopic extended right hemicolectomy was performed under general anaesthesia. The lesion was marked preoperatively allowing identification laparoscopically. There were no complications and the patient made an excellent recovery and was discharged home. He remains well at follow-up. Gross and Microscopic histological examination showed a submucosal lipoma with areas of fat necrosis and surface ulceration with extensive granulation tissue. This was distortion of the muscularis propria (Figures 3–5). Twelve lymph nodes showed reactive change only. The margins showed normal mucosa.

Polypoidal tumour measuring 4cm with an area of central ulceration

Gross slices of the tumour show adipose tissue expanding the submucosa. There are areas of fat necrosis and mucosal ulceration
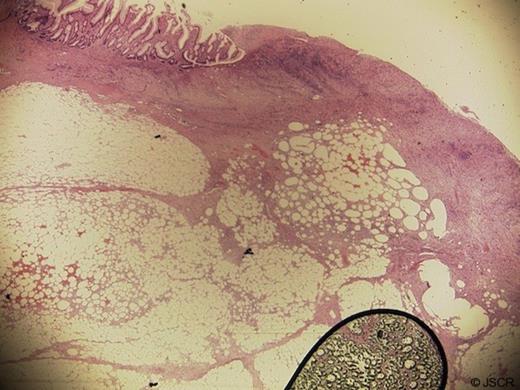
Microscopy shows lobules of mature adipocytes. There is extensive surface ulceration with underlying granulation tissue and areas of fat necrosis
DISCUSSION
Gastro-intestinal lipomas are rare and pose a diagnostic challenge. The endoscopic appearances may be worrying especially if ulceration has occurred. Imaging may reveal tissue with the signal and uptake of adipose tissue but a confident diagnosis may not be possible. Histology may be unhelpful due to the superficial nature of mucosal biopsies. Endoscopists, radiologists and pathologists need to be aware of this entity. Careful discussion and review of the investigations at an MDT meeting may permit a pre-operative diagnosis.
Endoscopic resection can be used where technically feasible but where doubt remains or this is not feasible then laparoscopic or open resection may be required.



