-
PDF
- Split View
-
Views
-
Cite
Cite
AJ Moss, D Valenti, SC Fraser, J Murie, An unusual shoulder injury, Journal of Surgical Case Reports, Volume 2011, Issue 10, October 2011, Page 9, https://doi.org/10.1093/jscr/2011.10.9
Close - Share Icon Share
Abstract
Traumatic pseudoaneurysm of the axillary artery is a rare sequel of shoulder injury. We report here a unique phenomenon of delayed presentation axillary pseudoaneurysm some time after an initial blunt injury, with no evidence of gross bony injury. The gentleman presented again some weeks later after a failure of rehabilitation and progressive neurological deficit in the affected arm. Ultimate management of the lesion was by endovascular insertion of a covered stent, and decompression of the axilla. Unfortunately the lack of subsequent neurological recovery parallels some of the findings in the literature, from cases where relief of the brachial plexus was not undertaken soon enough.
INTRODUCTION
Pseudoaneurysms of the axillary artery are uncommon and usually encountered after penetrating or blunt trauma to the axilla (1). In the latter case there tends to be an associated bony injury to the shoulder, most often an anterior dislocation (2), in which axillary artery damage has been reported at around 0.3% prevalence (3). Other injuries that have been described are fractures of the neck of the humerus and proximal humerus (4).
This pathology can lead to disastrous consequences if not suspected early (5). Indeed clinical suspicion can be lessened by the absence of hard initial signs of arterial injury (6) and the patient may present much later with potentially irreversible sequelae, particularly brachial plexus injuries (5).
Here we describe hare a unique case, where the patient initially presented with no dislocation or fracture and indeed the full consequences of the injury only became apparent when significant secondary neurological deficit had occurred.
CASE REPORT
An 80 year old man sustained an injury to his left shoulder during a fall. As a result of the intoxication the history of the mechanism of injury was poor. The gentleman was not taking aspirin or other anticoagulants. On examination movements of the shoulder girdle were reduced secondary to pain. Neurological examination of the left upper limb was normal, as was vascular state of the left arm. X-rays of the joint showed no bony injury (figure 1). Ultrasound showed a large periarticular haemarthrosis and an associated tear in the rotator cuff. Conservative therapy was adopted and the patient was discharged to the rehabilitation ward after two weeks.

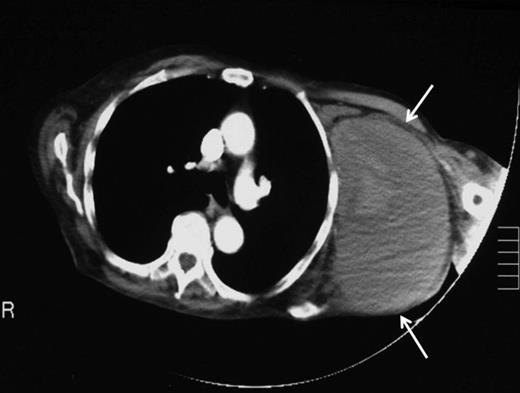
Ten weeks later a repeat orthopaedic review was requested by the rehabilitation team. There had been a slow onset and progression of oedema in the arm, with gradual progression of neurological deficit to the point at which the arm became useless and insensate. An increase in axillary bruising was noted. Also, the patient required a three-unit blood transfusion for a drop in haemoglobin six weeks after the injury. There was a thrill over the whole pectoral region and signs of venous hypertension in the arm. The left radial, ulnar and brachial pulses were normal. Repeat X ray showed subluxation of the left shoulder joint (figure 2). CT angiography revealed a distal axillary pseudoaneurysm with a sac of 15cm diameter (figure 3).

Repeat X-ray of left shoulder demonstrating subluxation of the head of the humerus
To attempt endovascular repair, an operative approach to the brachial artery preceded retrograde insertion of a 6cm long, 8mm thick Fluency nitinol self-expanding PTFE covered stent (Bard). This excluded the lesion successfully (figures 4 and 5). The haematoma was decompressed. Aspirin 75mg and clopidogrel 75mg were initiated for stent protection. The patient suffered a postoperative axillary wound infection which was treated successfully with antibiotics. There had been no recovery of neurological function in the arm. Neurophysiological studies revealed a proximal axonotmesis with a poor prognosis.

Angiographic localisation of the lesion in the third part of the axillary artery. Please note extravasation of contrast into the sac (arrows)

DISCUSSION
Pseudoaneurysms after blunt trauma to the shoulder tend to occur in the third part of the axillary artery (7). One theory for this is the lesser mobility of this region of artery because of the relatively fixed nature of the circumflex humeral and subscapular arteries, leading to tearing of the axillary artery with attempts at mobilisation (3,4). There are at least 27 reported cases in the literature of axillary pseudoaneurysm as a complication of anterior shoulder dislocation. We are unable to find any cases reported in the absence of a bony injury in blunt trauma.
In this case presentation was late with total paralysis of the arm secondary to a brachial plexus lesion. This has been described by several authors and can occur as a primary injury or delayed, as the aneurysm grows in size and compresses the plexus (8). The anatomical basis for this is likely the association of the axillary artery and cords of the brachial plexus in a common fascial sheath, the medial brachial fascial compartment (9). The secondary brachial plexus injury may be a neuropraxia (5) or an axonotmesis (8), the latter having significantly worse prognosis.
Delay decompression of paramount importance for recovery (1). In this case axonal degeneration was observed, with low likelihood of significant recovery. Six weeks post surgery, assessment by the rehabilitation team had not shown any sign of recovery. The poor outlook is supported by several authors, including Robbs et al (5), who reported 12 cases of delayed (after one to six weeks) compression of the brachial plexus by an axillary pseudoaneurysm in a variety of injuries. The outcome of the six patients presenting initially with total brachial plexus lesions were that none recovered fully, and one showed no recovery whatsoever at 18 months.
Clearly if a patient presents with signs of circulatory compromise of the upper limb or a wound very close to the anatomical location of a major artery there will be significant clinical suspicion of vessel injury. The problem in this case, as in others, is that none of these signs were present.
Several authors have highlighted important symptoms or signs in the early period post injury that can raise suspicion. In the study by Robbs (5) retrospective signs were found which would have aided diagnosis. These were: the prescence of significant bruising, swelling or a large haematoma; persistence of pain; a distal pulse deficit; onset of progressive neurological deficit; and a significant drop in haemoglobin or haematocrit. This is supported by the findings of other authors (1,4,6) Most of these observations were also made with this case. Perhaps the most significant and early finding in our patient was the large haematoma commented upon in the shoulder ultrasonographs.
The lesion was repaired by an endovascular retrograde approach whereby the neck of the lesion was located just distal to the origin of the subscapular artery and the cavity excluded successfully by the insertion of self-expanding Fluency nitinol PTFE-covered stent (Bard). Such a method was favoured here because the condition of the arm rendered open approaches hazardous. There are several reports of the treatment of such lesions by stent graft, including those of Xenos (10), whilst open repair also offers a simultaneous opportunity to explore for and deal with associated injuries.



