-
PDF
- Split View
-
Views
-
Cite
Cite
L Grainger, J Stammers, V Ranawat, A Loh, J Skinner, Delayed diagnosis of pseudoaneurysm formation in a patient with diaphyseal aclasis, Journal of Surgical Case Reports, Volume 2011, Issue 10, October 2011, Page 8, https://doi.org/10.1093/jscr/2011.10.8
Close - Share Icon Share
Abstract
A 15 year old boy, with known diaphyseal aclasis, presented with a swollen left leg. The diagnosis of popliteal pseudoaneurysm, a known and well understood vascular complication, was delayed due to presentation suggestive of a chondrosarcoma. In this age group, sarcomatous change is more common and a potentially sinister complication of diaphyseal aclasis. Following a sarcoma MDT referral, the correct diagnosis was confirmed by ultrasound and CT angiogram. This case identifies one of the largest, non-ruptured popliteal pseudoaneurysms reported and illustrates an unusual complication of a rare orthopaedic genetic condition, which is potentially limb threatening.
INTRODUCTION
Diaphyseal aclasis, also termed Hereditary Multiple Exostosis (HME) or osteochondromatosis is characterised by multiple bony prominences that grow near joint lines throughout the skeleton. These bony prominences, otherwise known as exostoses, can present as painless bony deformities or as a complication of the bony growth. (1)
There have been approximately 100 cases in the literature of vascular complications due to osteochondromas including pseudoaneurysm formation, occlusion, rupture or thrombosis. (2) This article describes the case of a 15 year old boy, with known HME, referred to the sarcoma MDT with a 9.5cm diameter mass in the popliteal fossa, confirmed by ultrasound as a delayed presentation of a pseudoaneurysm.
CASE PRESENTATION
A 15-year-old boy, with diaphyseal aclasis, presented with a two month history of a painful swelling in his left popliteal fossa, reportedly increasing in size. The patient also complained of paraesthesia distally. There was no night pain but the pain did prevent him from playing sports. He has had previous exostoses excised.
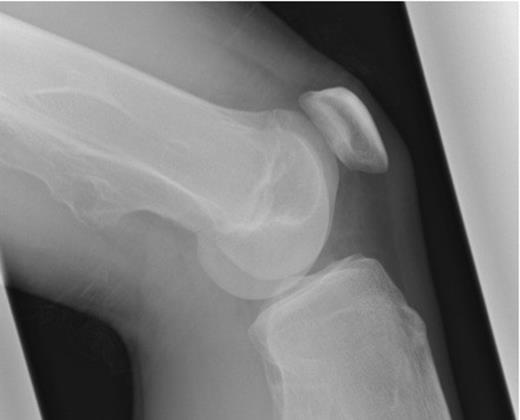
He presented to his local orthopaedic department where repeated radiographs (Figure 1) illustrated decreased cortical definition of the exostosis arising from the medial femoral metaphysis 15cm above the knee joint. There was no periosteal reaction but there was evidence of adjacent soft tissue swelling. At this point he was referred to the regional sarcoma MDT due to concern that the lesion had undergone malignant transformation.
On examination, there was a 10cm, non-tender, pulsatile mass in the popliteal fossa. The foot was warm with normal capillary refill, palpable posterior tibialis artery but absent dorsalis pedis. Sensation was present but reduced to the foot.
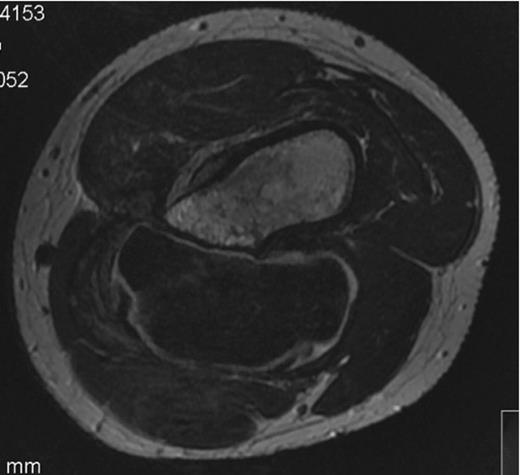
The MRI scan showed a lesion measuring 9.5cm in its greatest diameter, of uniform signal, with a cartilage cap exceeding 2cm throughout most of its surface. (Figure 2)
An ultrasound concluded an 8.8cm pseudoaneurysm and the patient was admitted for urgent pre-op CT angio (figure 3 and 4) and surgical exploration.

CT angiogram 3D reconstruction- Showing the bony exostoses and the popliteal aneurysm posterior to the right distal femur
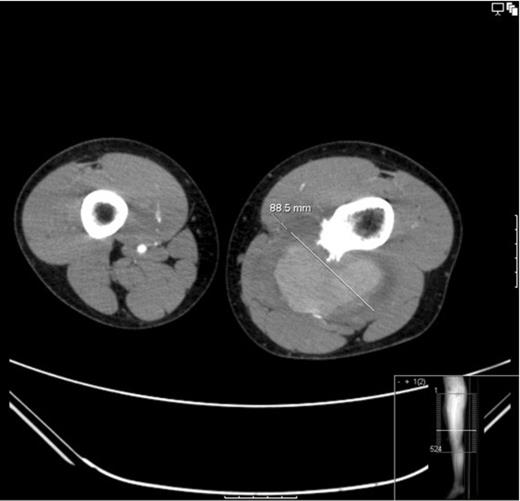
CT angiogram: Showing the diameter size of the aneurysm to be 88.6mm. The cross sectional image clearly shows the sharp bony exostoses that slowly eroded into the popliteal artery resulting in the pseudoaneurysm formation. The image also shows that the defect in the artery is still patent because the pseudoaneurysm is filling with contrast
The popliteal artery was explored. (Figure 5) The proximal popliteal artery was found to have a 1cm x 0.5cm wall defect adjacent to the bony exostosis. (Figure 6)The exostosis was excised and the 4cm of diseased artery repaired with end-to-end interpositional long saphenous vein graft. (Figure 7)


Intraoperative Photograph showing the 1cm x 0.5cm defect in the popliteal artery wall caused by the sharp bony exostoses

Intraoperative Photograph showing the end to end interpositional long saphenous vein graft
Post operatively the patient recovered without complication. Histology confirmed an osteochondroma with no malignant cells and vessel consistent with pseudoaneurysm formation. He was followed up with an ultrasound Doppler after 6 weeks demonstrating a patent vein graft and will undergo local vascular follow-up. His 6 month post-operative check-up revealed no complications but he will have regular follow-up for any painful, rapidly growing exostosis associated with his hereditary condition.
DISCUSSION
Diaphyseal aclasis is a rare genetic skeletal condition due to developmental abnormalities of the growth plate causing multiple cartilage covered exostoses to form on the surface of the metaphysis or the adjacent diaphysis region of long bones. Diaphyseal aclasis is usually diagnosed in childhood however it is believed that radiologically the exostoses are present since birth. (3)
Vascular complications of the popliteal vessel occur due to ossification of the previously protective cartilage cap, around the 2nd decade and relative immobility of the artery in the popliteal fossa between exiting Hunter’s canal and the trifurcation. (4) The artery undergoes chronic abrasion on the sharp exostosis forming a defect in the adventitia resulting in pseudoaneurysm formation. (5)
It is controversial whether exostoses that lie near a vascular axis should be removed on identification to prevent vascular compromise from occurring. Considering most exostoses are innocent, most authors suggest that surgical excision is only required when complications have occurred or malignant transformation is suspected. If preventative surgery is not performed, regular ultrasound Doppler scans should be performed in order to screen for complications. (6)
In addition to vascular complications, bony exostosis can also present acutely with nerve compression, bursitis due to bony irritation, stalk fracture or necrosis of the cartilaginous cap following infarction. (7)
Due to the acute presentation of this vascular complication there was no time for pre-operative tissue diagnosis, which would be routinely performed. It was important that the procedure was performed by an experienced orthopaedic tumour surgeon to ensure adequate margins were achieved. Recent studies report a lifetime risk of sarcomatous transformation in single lesions of approximately 1% but up to 5% in HME. (8) The majority are chondrosarcomas, however, osteosarcomas and malignant fibrous histiocytomas have been reported.
Concerning features that warrant further investigation include:
A rapidly enlarging mass, particularly in those beyond skeletal maturity
Shoulder girdle and pelvic exostosis (9)
Cartilage capsule exceeding 1.5cm
Investigation with ultrasound, MRI and image guided or open biopsy is advocated if an exostosis has concerning features. There are recent studies advocating PET/CT imaging to monitor known benign exostosis for malignant transformation. (10) Due to the relative rarity of these lesions it is important to review the images and histology in a specialised bone tumour multi-disciplinary meeting.
This case illustrates a late presentation of a known complication associated with diaphseal aclasis. In this age group we present one of the largest, non-ruptured, popliteal pseudo aneurysms reported. It is important to maintain a high index of suspicion of an increasing soft tissue lesion due to the risk of sarcomatous transformation in patients with MHE; however, this focus delayed earlier presentation to vascular surgeons putting the patient at risk of a limb threatening rupture.



