-
PDF
- Split View
-
Views
-
Cite
Cite
Nadia C Sciberras, James R Lindsay, A rare presentation of TB: Osteomyelitis of distal ulna, Journal of Surgical Case Reports, Volume 2011, Issue 1, January 2011, Page 4, https://doi.org/10.1093/jscr/2011.1.4
Close - Share Icon Share
Abstract
Tuberculosis (TB) is a major health issue in both developing and developed countries such as the UK. Healthy individuals who contract the infection have only 5-10% chance of converting to the active disease over their lifetime. We present the clinical history of a 76 year old female who attended the emergency department complaining of wrist pain, and was only diagnosed with TB after three years. This case report emphasises the importance of including TB in the differential diagnosis when treating patients with an infection resistant to conventional antibiotics, even though risk factors for TB may not be evident or special stains for TB are negative.
INTRODUCTION
Tuberculosis (TB) is a major health issue in developing countries with over two billion people being infected with tuberculosis bacilli world wide (1). Although TB was recently regarded primarily as a disease of the developing countries it is now also on the increase in developed countries such as the United Kingdom, mainly as a result of globalisation as well as an increase in immunosuppressed patients. Figures by the Health Protection Agency (HPA) show that the cases of TB in the UK increased by 5.5% in 2009 when compared to those in 2008 (2).
CASE REPORT
This Caucasian patient presented to the emergency department with sudden pain localised to the ulnar aspect of her wrist. There was no history of recent trauma. She had slight swelling of her wrist and was tender over the distal ulna. X-ray of the forearm was normal and she was treated conservatively but was lost to follow up.
She presented again at the orthopaedic clinic 26 months later with continuing swelling and pain. Ultrasound showed a synovial tumour on the dorso-medial aspect of the wrist (Figure 1). Aspiration of the cyst produced a small amount of pus. She was admitted for incision and drainage of the abscess. Microscopy of the tissue showed a granulomatous inflammation.
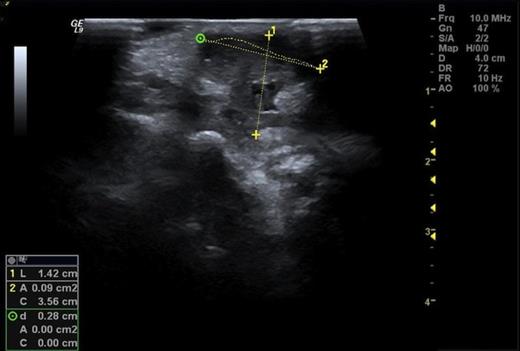
Ultrasound showing a synovial tumour on the dorsal medial aspect of the wrist
However, special stains for fungi and acid fast bacilli were negative. Subsequently the patient developed a sinus and continued to have a chronic discharge from her left wrist. Repeated wound swabs did not yield any growth.
She was subsequently referred to the hand clinic. X ray this time showed destruction of the ulnar styloid consistent with a bony infection (Figure 2). MRI showed destruction localised around the ulnar head with oedematous changes extending up the shaft of the ulna (Figure 3).

AP Xray of the wrist showing destruction of the ulnar styloid consistent with a bony infection. Soft tissue swelling can also be noted over the dorsum of the wrist
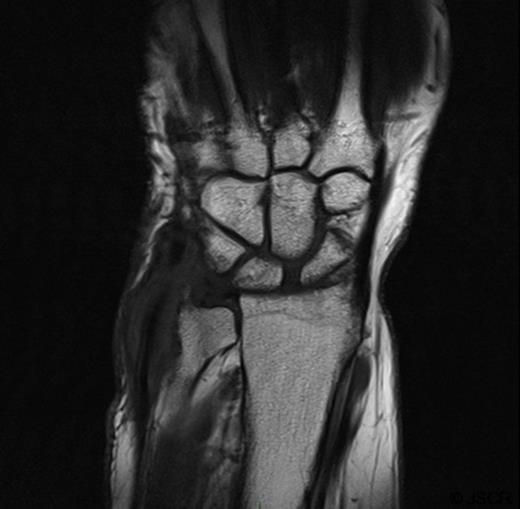
MRI showing localised destruction around the ulnar head. The MRI also shows thickening around the extensor carpi ulnaris tendon in keeping with marked tenosynovitis at this site.
The patient agreed to a repeat biopsy and excision of the necrotic bone (Figure 4). Microscopy of the specimen again showed a florid granulomatous inflammatory process with areas of fibrinoid necrosis. Cultures isolated Mycobacterium tuberculosis.

Post-operative Xray of the wrist showing excision of the ulnar styloid
Further enquiry revealed that our patient had been experiencing lethargy but no other features to suggest tuberculosis. Blood investigations, as well as her chest x ray, were normal. Following the diagnosis of TB, the patient recalled that in her former post as a nursing assistant, when she was much younger, she was exposed to patients with TB. Anti-tuberculous treatment resulted in complete resolution of the patient’s symptoms.
DISCUSSION
Tuberculosis is one of the oldest diseases known to man. Although improvements in its management and treatment are continuously occurring an estimated 1.8 million people died of TB in 2008 (1). Extra-spinal tuberculous osteomyelitis is rare and comprises about 2-3% of all cases of osteoarticular tuberculosis, with the hip and knee joints being the most common following spinal involvement (3). Tuberculous involvement of the ulna is uncommon and tends to be more common in the diaphysis.
A high index of suspicion of TB is important to obtain the correct diagnosis. In chronic soft tissue and bony infection not responding to conventional antibiotics TB should be excluded. The diagnosis of TB may not be evident from the history and examination and indeed no obvious risk factors may be present as in our case.
In our patient the infection could have been contracted at a much younger age, when she was caring for patients infected with tuberculosis, and remained latent. However no other risk factors were evident that could explain why the disease was activated after such a long period of latency. It is also interesting to note that the actual distal radio-ulnar joint was not involved, most of the destruction being situated around the ulnar process. Although localisation of the tuberculous infection in the bone without joint involvement can occur, this is rare (3).



