-
PDF
- Split View
-
Views
-
Cite
Cite
AC Coombs, Ameloblastoma of the frontal sinuses: a rare site for recurrence, Journal of Surgical Case Reports, Volume 2011, Issue 1, January 2011, Page 2, https://doi.org/10.1093/jscr/2011.1.2
Close - Share Icon Share
Abstract
Ameloblastoma is a benign odontogenic tumour which commonly recurs after initial surgery; most recurrences occur at the site of the primary tumour. A rare case of recurrence of a maxillary ameloblastoma in the frontal sinuses is presented. To our knowledge there are no previous reports in the literature of a benign maxillary ameloblastoma extending into the frontal sinuses.
INTRODUCTION
Ameloblastoma is a benign, locally aggressive tumour which arises from odontogenic epithelium and is associated with a high recurrence rate. It is the second most common odontogenic tumour but is still relatively rare, accounting for only 1% of all tumours that arise in the mandible and maxilla. (1) Both sexes are affected equally and the median age at presentation is 36 years. (2)
Although slow-growing, ameloblastomas are locally invasive. Maxillary ameloblastomas and the solid/multicystic variant are more likely to spread, making complete clearance more difficult and thus increasing the recurrence rate. Management by radical resection has led to an improved cure rate but recurrences still occur and may present many years after primary surgery. (3)
A case of a maxillary ameloblastoma with an unusual initial presentation of nasal obstruction and with recurrence after radical surgery in the frontal and ethmoid sinuses is described. No cases could be found in the literature of extension of a benign maxillary ameloblastoma into the frontal sinuses.
CASE REPORT
A 44-year-old man was referred to the ENT Department at the John Radcliffe Hospital, Oxford in May 2009 because of a possible recurrence of an ameloblastoma.
He had originally presented in 2006 with a three year history of worsening left-sided nasal obstruction. Examination revealed a left-sided nasal polyp with pink, friable mucosa. Biopsy of the nasal polyp showed ameloblastoma with a follicular and plexiform pattern and a computed tomography (CT) scan revealed this to be secondary extension of a left maxillary ameloblastoma. He underwent a left maxillectomy in May 2007. Histology showed complete excision of an ameloblastoma of the posterior maxillary bone with minimum clearance margins of 5mm.
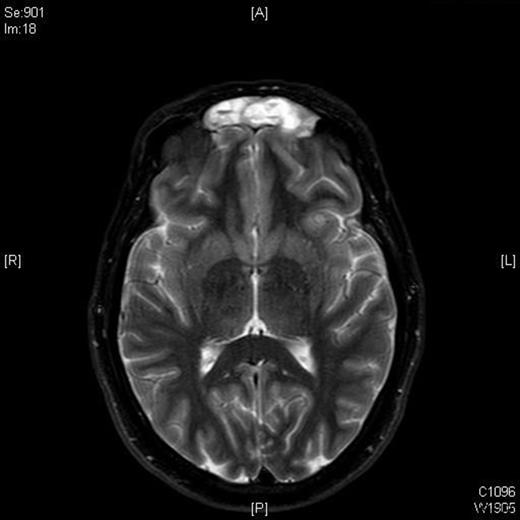
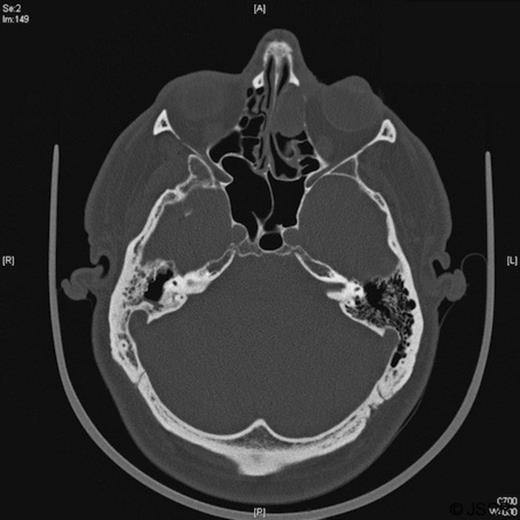
A follow-up MRI scan in 2009 showed contrast-enhancing soft tissue abnormalities within both of the frontal sinuses and the left ethmoid sinus (Figures 1 and 2). A CT scan showed soft tissue abnormalities in these locations (Figure 3). An incisional biopsy confirmed a subepithelial ameloblastoma.

In January 2010 a frontoethmoidectomy with an osteoplastic flap was performed to remove the tumour. Macroscopically, there was a light-brown polypoid tumour in the sinuses and microscopically this was confirmed to be a solid/multicystic ameloblastoma with no evidence of malignant transformation. The patient made a good recovery after surgery and will receive follow-up imaging to check for further recurrence.
DISCUSSION
Ameloblastomas arise from residual epithelial elements of tooth development: dental lamina, enamel organ, lining of odontogenic cysts or the basal cells of the oral mucosa. (4) The majority occur in the mandible and the maxilla, with the occurrence in the mandible being five times higher than in the maxilla.
There are four types of ameloblastoma: solid/multicystic (92% of ameloblastomas), unicystic, desmoplastic and peripheral. (5) The term ‘malignant ameloblastoma’ is used if the primary tumour shows any features of malignancy (e.g. increased mitotic activity) or if there is metastatic growth.
The usual clinical presentation of ameloblastoma is an asymptomatic, slow-growing intraoral or facial swelling or as an incidental finding on dental radiographs. Less commonly, patients may present with loosening of teeth, pain, malocclusion or, if the maxilla is affected, epistaxis or nasal obstruction. (4)
There are no pathognomic radiological features of ameloblastoma, but radiographs may show a well-defined radiolucent lesion with scalloped margins which may be unilocular or multilocular (‘soap bubble’ appearance). CT scans provide further information on the extension and MR scans demonstrate the components of the tumour in greater detail. (6) Diagnosis is histological: the ameloblastoma is composed of nests, strands and cords of odontogenic epithelium, separated by fibrous connective tissue (1).
Although histologically benign, ameloblastomas are locally invasive and have high recurrence rates, often many years after initial surgery. The anatomical site, clinicopathological variant and the treatment modality affect the rate of recurrence. Maxillary ameloblastomas have five times the recurrence rate of mandibular tumours. The thin bone of the maxilla allows relatively unimpeded spread to surrounding tissues, in contrast to the thick cortical bone of the mandible. The solid/multicystic variety has the greatest propensity for local infiltration and therefore recurrence, with the actual margins of the tumour often extending beyond its apparent clinical or radiographic margins. (4) The use of curettage to treat maxillary ameloblastomas is associated with a very high recurrence rate and therefore radical resection with margins of 10-15mm is the current recommended treatment of maxillary tumours. (7)
Ameloblastoma of the sinonasal tracts is uncommon and of the frontal sinus is very rare. A Medline search was performed using different combinations of the key words ameloblastoma, odontogenic tumours, adamantinoma, sinus, sinonasal, frontal sinus. This search found that ameloblastoma affecting the sinonasal cavities is most commonly due to extension of a maxillary tumour. (8,9) There are case reports of extremely rare primary sinonasal ameloblastomas but no previous reports were found of extension of a benign maxillary ameloblastoma into the frontal sinuses, as in this case. (10)
There are two hypotheses for this recurrence in the left ethmoid and frontal sinuses. The initial surgery may have failed to completely remove all the tumour as the resection margins were only 5mm in some places and residual tumour may have subsequently invaded up into these sinuses. Alternatively, the ameloblastoma may have already invaded up towards or into these sinuses at the time of initial presentation, but such invasion was too microscopic to be detected on the initial imaging. The intervening two years allowed these foci of ameloblastoma to grow to detectable sizes.
This case reinforces that maxillary ameloblastoma is a locally aggressive tumour that can invade surrounding structures. It is therefore important to investigate patients for such invasion and to ensure wide, clear resection margins. This case also highlights the importance of regular follow-up as recurrences can occur in unusual locations and varying periods of time after surgery.



