-
PDF
- Split View
-
Views
-
Cite
Cite
AA Sheikh, J Watt, M Tee, CR Selvasekar, Appendicitis as a complication of colonoscopy, Journal of Surgical Case Reports, Volume 2010, Issue 9, November 2010, Page 1, https://doi.org/10.1093/jscr/2010.9.1
Close - Share Icon Share
Abstract
Acute appendicitis is an extremely rare complication of colonoscopy, with no reports in the British literature. Here we discuss a case report of a patient who developed acute appendicitis 24 hours following a normal diagnostic colonoscopy. This case report highlights the rarity of this life threatening complication and discusses its aetiology.
INTRODUCTION
Acute appendicitis following a diagnostic colonoscopy is exceedingly rare with only 12 reported cases in the literature none of which are from the United Kingdom (1-3). Moreover, only one case report describes perforated appendicitis following colonoscopy, making this a life threatening complication (1). The British Society of Gastroenterology recognizes most rare complications of colonoscopy however, does not make reference to appendicitis as a recognized complication owing to it extremely rare occurrence (4). The usual pathogenesis of appendicitis involves obstruction of the lumen with a faecolith resulting in increased intraluminal pressure, impaired blood flow and inflammation. Lymphoid hyperplasia, barium remnants, foreign bodies and parasites are known to block the appendicular lumen, leading to acute appendicitis (3). Here we present a case of perforated appendicitis 48 hours following a diagnostic colonoscopy.
CASE REPORT
A 50 year old woman attended a diagnostic colonoscopy following a recent history of fresh rectal bleeding with a background of colonic polyps which had previously been removed endoscopically with no subsequent complications. She presented as an emergency 24 hours following a normal colonoscopy with a macroscopically normal caecum and appendicular orifice. Her symptoms were of abdominal pain 4 hours following the procedure with nausea and absence of bowel movement since her procedure. Clinically her observations were haemodynamically normal other than a pyrexial at 38.1° C with rebound tenderness in the right iliac fossa. Her inflammatory markers were raised; white cell count was 17.8 x 109 cells/L with neutrophilia, CRP was 95 mg/L. No free intraabdominal air was identified on erect chest x-ray and the abdominal film showed a few dilated small bowel loops. Suspecting a colonic perforation the patient was admitted and treated with intravenous antibiotics.
The CT scan of her abdomen did not reveal any free intraperitoneal gas however suggested inflammatory changes in the terminal ileum, caecum and ascending colon with mural thickening. The features reported were not typical of acute appendicitis but indicated possible active Crohns disease (Figure 1). As her clinical and haematological parameters did not improve with conservative treatment, a diagnostic laparoscopy after 48 hours was performed. Intraoperative findings were of free fluid in the pelvis and an inflammatory mass involving the terminal ileum with a perforated, grossly inflamed appendix. The patient underwent a laparoscopic appendicectomy and made an uneventful recovery being discharged home a few days later.
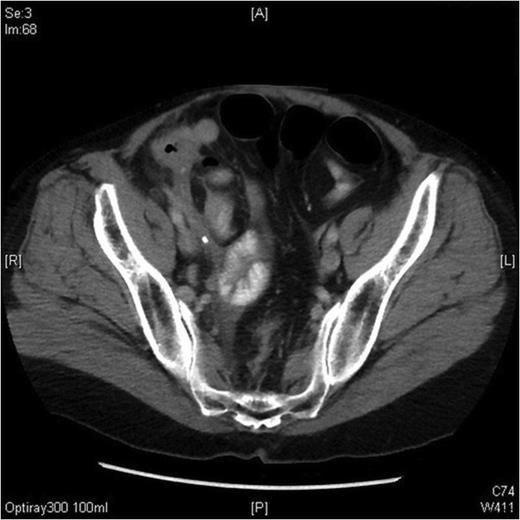
CT scan demonstrating the presences of inflammation in the right iliac fossa, with some distension of the appendix tip
DISCUSSION
Colonoscopy is a relatively safe procedure with well recognized complications of bleeding and perforation, moreover rare occurrences such as are splenic injury, pneumomediastinum, pneumothorax, incarcerated hernia, ileus and diverticulitis are described in the literature (1,2,4). Abdominal pain following colonoscopy is commonly attributed to retained gas or colonic spasm.(3). Additionally, distinguishing appendicitis from post-polypectomy syndrome, which is a combination of pain, peritoneal irritation, leukocytosis with fever can be challenging. CT scan certainly has a role in diagnosis, however is often limited in the early stages owing to the lack inflammatory changes.
The suggested pathogenesis is excess pressure from the endoscope at the appendiceal orifice supplemented with barotrauma secondary to excess inflation resulting in inflammation and occlusion of the appendiceal lumen which could be in the background of subclinical disease (1). Occlusion of the lumen has been reported following impaction with stool caused by the colonoscope, leading to increased intraluminal pressure, impaired blood flow and inflammation. Other cases reported in the literature suggest the onset of symptoms post procedure with two cases using colonoscopy to diagnose atypical appendicitis (5).
Our patient did not have concurrent coincidental appendicitis, as the appendiceal orifice visualized at colonoscopy was normal along with the caecum and terminal ileum indicating no evidence of inflammatory bowel disease. Appendiceal orifice was not intubated making direct luminal trauma unlikely however barotraumas due to insufflation is a possibility likewise introduction of stool into the appendix could have been a possibility.
Although the exact aetiology is unclear the diagnosis of appendicitis following colonoscopy can be challenging and hence prompt recognition of this complication should be considered as early intervention can lead to uncomplicated outcomes.



