-
PDF
- Split View
-
Views
-
Cite
Cite
Seong K. Lee, Eddy Carrillo, Andrew Rosenthal, Rafael Sanchez, Antonio Pepe, Neil Abrahams, Behruze Ruyani, Perinephric Capsular Haematoma Associated with Complicated Pyelonephritis in a Patient with HIV, Journal of Surgical Case Reports, Volume 2010, Issue 8, October 2010, Page 2, https://doi.org/10.1093/jscr/2010.8.2
Close - Share Icon Share
Abstract
A 53 year-old-male patient presented with 24 hours of left flank pain. He was an undiagnosed HIV positive individual with no history of trauma. He was anaemic and in acute renal failure with a serum creatinine of 4.14 mg/dL. A CT scan demonstrated a left perinephric capsular haematoma with retroperitoneal stranding. Due to haemodynamic instability, the patient was taken to the operating room and a nephrectomy was performed. Post-operatively, the patient required temporary haemodialysis. Pathologic examination of the specimen demonstrated active infection with a haematoma surrounding a fistulous tract communicating with the capsular surface. Infection is a rare cause of non-traumatic capsular hematomas of the kidney.
INTRODUCTION
Capsular haematoma of the kidney may occur from many causes including trauma, tumour, coagulopathy, ruptured cyst or vascular malformation (1). Infection has only rarely been reported in association with a spontaneous rupture or capsular hematoma (2). In the following case, we describe a patient with undiagnosed HIV who presented with a perinephric capsular haematoma associated with complicated pyelonephritis.
CASE REPORT
A 53 year-old-male patient with a history of diabetes and undiagnosed HIV presented with 24 hours of back and left sided abdominal pain. There was no history of trauma. On physical exam the patient had a distended abdomen and was moderately tender to palpation. He was found to be anemic with a haemoglobin and haematocrit of 7.2 gm/dL and 21%, respectively. In addition, the patient’s serum potassium was 7.7 mmol/L and he was in acute renal failure with a BUN of 59 mg/dL and serum creatinine of 4.1 mg/dL. The most recent laboratory values two years prior revealed a BUN and Cre of 15 mg/dL and 1.0 mg/dL, respectively. A computerised tomography scan of the abdomen and pelvis demonstrated a large left sided perinephric capsular haematoma without other significant abnormalities of the kidney (Figure 1). The patient was admitted to Intensive Care Unit for resuscitation and treatment of the hyperkalemia. Despite transfusion of packed red blood cells and correction of the serum potassium (4.9 mg/dL), the patient remained haemodynamically unstable and was subsequently taken to the operating room for an exploratory laparotomy.
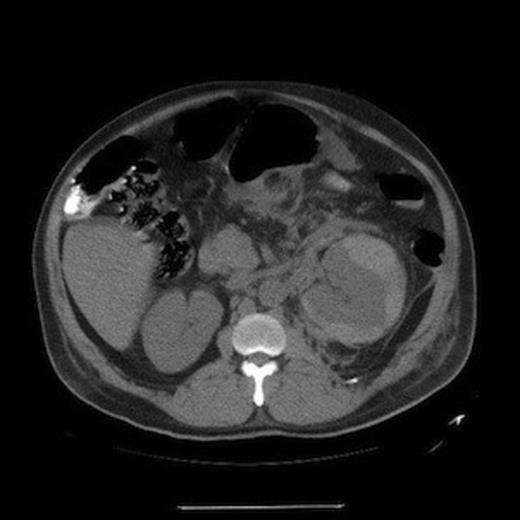
CT scan of abdomen demonstrating a left perinephric capsular hematoma with retroperitoneal stranding
During the operation, the retroperitoneum was explored and the kidney revealed a large capsular haematoma with a necrotic area (3 x 4 cm) over the surface of the kidney (Figure 2). The abdomen was otherwise unremarkable and a nephrectomy was performed due to the patient’s condition and the abnormal capsule. Post operatively, the patient remained in anuric renal failure and developed respiratory failure requiring a tracheostomy. He required renal replacement therapy with intermittent haemodialysis. He slowly recovered and after approximately four months he was weaned off haemodialysis with a baseline BUN and creatinine of 50 mg/dL and 1.69 mg/dL. During this time, laboratory studies were performed which revealed the patient was Hepatitis B surface Ag positive and a subsequent HIV test was also found to be positive. His absolute CD4 count was only 9 per microlitre.

Gross specimen following removal demonstrating a ruptured necrotic capsule (arrow)
Pathologic examination of the removed kidney demonstrated active infection with bacteria and microabscess (Figure 3). In addition, the granulomatous and necrotising inflammation seemed to coalesce in a fistulous tract toward the renal capsular surface with a surrounding haematoma (Figure 4). Delayed review of the slides following the discovery of his HIV status demonstrated classic focal segmental glomerulosclerosis.
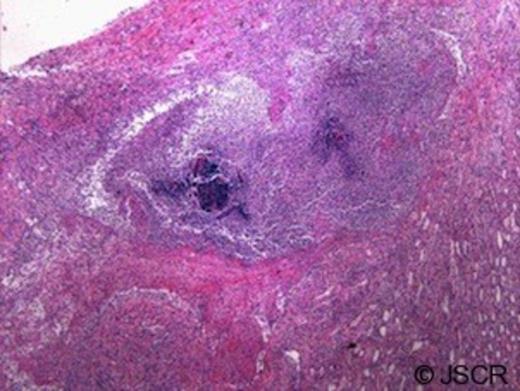
Renal medulla with bacteria, microabscess, and neutrophil reaction (10x magnification)
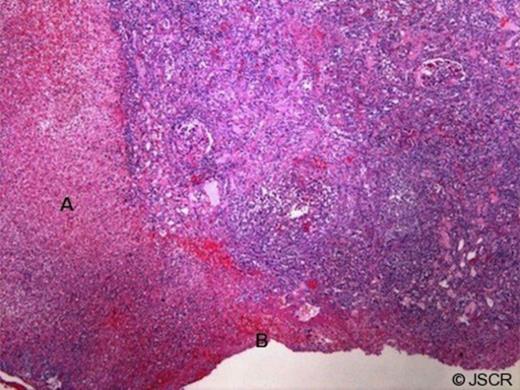
Cortex with necrosis, hemorrhage and fistulous tract (A) associated with capsular hematoma (B) (10x magnification)
DISCUSSION
Underlying abnormalities to the kidney should always be suspected in cases of spontaneous perinephric capsular haematoma due to the high incidence of associated tumours or other pathology (1). Infection has only rarely been reported in association with a perinephric haematoma (2). We report a case in a patient with an unknown diagnosis of HIV who presented with a spontaneous haematoma due to severe complicated pyelonephritis. The patient’s initial hypotension was likely explained by his profound anaemia. However, the fact that the patient did not respond appropriately to resuscitation and transfusion may be partially explained by sepsis and severe acute infection. Regardless, the patient improved clinically following surgery and his post-nephrectomy renal failure ultimately improved and he was able to be weaned off renal replacement therapy. While sepsis, abscess, renal failure and chronic infection are all well known complications of pyelonephritis, capsular haematoma and rupture has been only rarely described, and not previously reported in a patient with HIV.



