-
PDF
- Split View
-
Views
-
Cite
Cite
Valerie Sams, Khanjan H Nagarsheth, Todd A Nickloes, Transorbital Penetrating Intracranial Injury Caused by Sheppard’s Hook, Journal of Surgical Case Reports, Volume 2010, Issue 7, September 2010, Page 3, https://doi.org/10.1093/jscr/2010.7.3
Close - Share Icon Share
Abstract
Intracranial injury resulting from transorbital penetrating objects is rare in a noncombat setting. As such there is a significant lack of data pertaining to the management of non-projectile traumatic brain injuries due to foreign bodies entering the brain. Intracranial complications can include intracerebral hematoma, cerebral contusion, intraventricular hemorrhage, pneumocephalus, brain stem injury, and carotid cavernous sinus fistula. This is the first report of a transorbital penetrating intracranial injury caused by a Sheppard’s hook, which was managed utilizing a multi-disciplinary, non-operative approach.
INTRODUCTION
Intracranial injury resulting from transorbital penetrating objects is rare in a noncombat setting. As such there is a significant lack of data pertaining to the management of non-projectile traumatic brain injuries due to foreign bodies entering the brain. It is pertinent to understand the mechanism of injury, anatomy of injury, and treatment of such injuries. This is the first report of a transorbital penetrating intracranial injury caused by a Sheppard's hook, which was managed utilizing a multi-disciplinary, non-operative approach.
CASE REPORT
The patient was a 52 year old female who presented to the trauma bay of the University of Tennessee Medical Center-Knoxville via helicopter after suffering a fall. The patient admitted to falling onto a Sheppard-hook planter device while gardening. She denied any loss of consciousness, having dialed 911, for emergency services, herself after pulling the Sheppard-hook out of the ground and carrying it into her home. She presented with a Glascow Coma Scale score of 15, hemodynamically stable and had no other injuries. Her right eye had significant edema and could not be examined; however, the hook appeared to enter the orbit beneath the inferior eyelid, below the globe and through the roof of the orbital fossa (Figure 1).

After obtaining a four view skull series x-ray (Figure 2), it became evident the object traveled through the right orbital fossa superiorly, with the tip projecting over the medial right frontal lobe anterior to the pituitary, fracturing the posterior supero-medial orbital wall. Secondary to the size of the object, and with the assistance of emergency medical services and the fire department, the patient was taken outside to the ambulance bay where a plasma saw was utilized to separate the hook from the stanchion post in preparation for removal (Figure 3).


In consultation with neurosurgery, ophthalmology and oral maxillofacial services, it was decided to intubate the patient and remove the object, with a CT scan of the head to follow immediately upon removal. After adequate sedation and intubation, and with continued stabilization of the head and cervical spine, the Sheppard’s hood was removed by pulling in a rotational motion along the natural curve of the hook. There was a minimal amount of bleeding from the orbit, and a pressure dressing was applied.
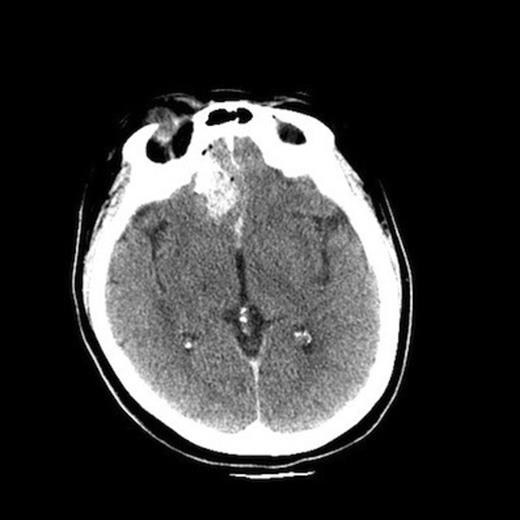
Upon removal of the hook, the patient was taken immediately to the CT scanner for a CT angiogram of the head. The CT scan demonstrated some leftward deviation of the anterior cerebral arteries, but there was no evidence of vascular injury or active hemorrhage. There was evident some recent parenchymal and subarachnoid hemorrhage with small subdural hygroma over the right frontal convexity. There was also hemorrhage and edema of the inferior orbit with displaced medial right orbital wall fracture. The globe was slightly dysmorphic, although the lens was intact, and there was no gross evidence of intraocular hemorrhage. The right orbit extruded such that 75% was beyond the orbital rim (Figure 4). A repeat CT scan was obtained two hours later which demonstrated no change and that the injury was stable.
The patient was admitted to the intensive care unit, weaned from the ventilator, and extubated without incident the following morning. Upon extubation the patient complained of a slight headache and right eye pain. She was transferred to an acute care floor the following day. A final CT scan demonstrated slight improvement of the intracranial and orbital findings. The patient was discharged to home with no apparent neurological deficits or personality changes per her own admission, and per her family. The patient was seen in the outpatient clinic approximately one week after discharge doing well, and without evident sequelae. Ophthalmology determined her globe and lens to be intact, and felt she would suffer no untoward effects of the injury once her edema resolved, with only a slight loss of visual acuity. Neurosurgical follow up three weeks post-injury revealed no complications associated with the injury. Oral maxillofacial follow-up likewise revealed no evident difficulties.
DISCUSSION
Transorbital penetrating brain injury secondary to a non-projectile foreign body is a rare incident. Intracranial complications can include intracerebral hematoma, cerebral contusion, intraventricular hemorrhage, pneumocephalus, brain stem injury, and carotid cavernous sinus fistula. Infection is a later complication that has to be kept in mind. The direction of the penetration is the major determinant of what type of injury will occur. If the penetration is parallel to the orbital roof, it will violate the cranium through the superior orbital fissure or optic canal, and usually does not result in bone fracture. If the penetration runs upward, the orbital roof is thin and will be easily fractured causing penetration of the frontal lobe, leading to intracerebral hematoma. Patients with these types of injuries actually have a favorable prognosis, and the treatment of removal with follow up CT and observation is usually sufficient. As Kasamo et al. demonstrated, a “pull and see” method as treatment policy has favorable outcomes.(1) If the object is completely intracranial or lodged such that it cannot be removed easily, frontal craniotomy is an effective surgical approach.(2) According to a report by Farhadi et al. a surgical treatment standard has not yet been determined; however, a rational treatment strategy should focus on preventing further brain damage. (3) Transorbital penetrating brain injuries are treated best utilizing all up-to-date technical developments, including intraoperative CT-scanning, to increase the safety if there is a risk of immediate life-threatening intracranial bleeding.
Liu et al. found in their review of 28 transorbital intracranial foreign body cases that the relationship between the foreign body and vascular structures such as the internal carotid artery should be examined carefully before extraction. (4) We were able to review the skull series with a radiologist and a neurosurgeon and based on known anatomy were able to conclude that in our case it was unlikely that this had violated any major vascular structure. Their review also found that direct extraction of foreign bodies causes less injury when compared to more extensive surgical techniques. This is consistent with the aforementioned method of “pull and see” described by Kasamo et al. (1) It is important to note that managing an injury as the one described here should only be undertaken at a level one trauma center where all the necessary consulting services and facilities are readily available to assure the best possible patient outcome. The patient’s Glascow Coma Scale score should be assessed on arrival and then airway secured by the appropriate team if necessary. Following this, CT angiography is probably the single best radiographic study to evaluate any kind of major vascular injury, which if present would alter management of this injury. Finally, lessons from combat zones have taught us that there is a significant relationship between combat ocular trauma and traumatic brain injury (TBI) such that nearly two thirds of patients with ocular trauma have traumatic TBI and ocular trauma is a common finding in all TBI. (5)
The preceding describes the presentation and management of a transorbital penetrating brain injury. It is important to note that a multi-disciplinary approach was utilized in order to remove the foreign body with minimal risk. This was done in order to obtain the best possible outcome. It is crucial for the trauma team take full advantage of the resources available and co-ordinate the multiple consultants and local rescue crews to aid in any patient’s care.



