-
PDF
- Split View
-
Views
-
Cite
Cite
Oladejo Olaleye, Matthew Oliver, Helmut Zahn, External iliac vein compression and thrombosis by a migrated acetabular screw following total hip arthroplasty, Journal of Surgical Case Reports, Volume 2010, Issue 3, May 2010, Page 5, https://doi.org/10.1093/jscr/2010.3.5
Close - Share Icon Share
Abstract
A fifty-nine year old gentleman underwent a right total hip replacement in another hospital for protrusio osteoarthritis of the right hip. Post-operatively he developed a large right-sided ilio-femoral deep venous thrombosis. A pelvic radiograph showed that the acetabular construct had migrated medially into the pelvis with a CT scan showing compression of the external iliac vessels by one of the acetabular screws. Revision surgery was carried out in collaboration with the vascular surgeons. This case report highlights the importance of pre-operative planning to avoid medial wall perforation in patients with protrusio osteoarthritis. It also illustrates an unusual complication of compression of the external iliac vessels causing massive ilio-femoral thrombosis.
The management of this potentially limb threatening complication is described in this case report.
INTRODUCTION
Protrusio acetabuli should be recognized prior to hip replacement surgery as this helps avoid potential complications. This case report reiterates this fundamental principle as it highlights migration of the acetabular construct following over-reaming in a patient with protrusio acetabuli. This led to massive ilio-femoral thrombosis and eventual complex revision surgery
CASE REPORT:
A fifty-nine year old gentleman with protrusio osteoarthritis of both hips was scheduled for a right total hip replacement. He had been made redundant from his occupation as a woodcutter because of the severity of his osteoarthritis. His operation was carried out using the modified Hardinge approach to the hip joint.
He was admitted to our hospital four days after discharge, with a painful swollen right leg. A Doppler ultrasound scan of his right leg confirmed a large ilio-femoral deep vein thrombosis. He was commenced on therapeutic low molecular weight heparin. He continued to complain of pain in his right leg without resolution of the pitting oedema.
A post-operative radiograph (Figure 1) revealed medial migration of the acetabular construct prompting CT scans of his pelvis.

A pelvic radiograph showing migration of the acetabular construct
The acetabular screws were seen projecting medially into the pelvis with the anterior screw closely abutting the external iliac artery and vein causing compression (Figure 2).

A CT Scan of the pelvis showing compression of external iliac vein by acetabular screw
He subsequently underwent a revision of his right total hip replacement. The procedure was carried out together with a vascular surgeon. A right sided extra peritoneal approach to the right iliac vessels was performed. The iliac vessels, which had been compressed by the displaced acetabular cup and screws, were secured with vascular slings.
To avoid thrombus escaping from the iliac vein at the time of revision, a vena cava filter was inserted from the contralateral femoral vein (Figure 3).
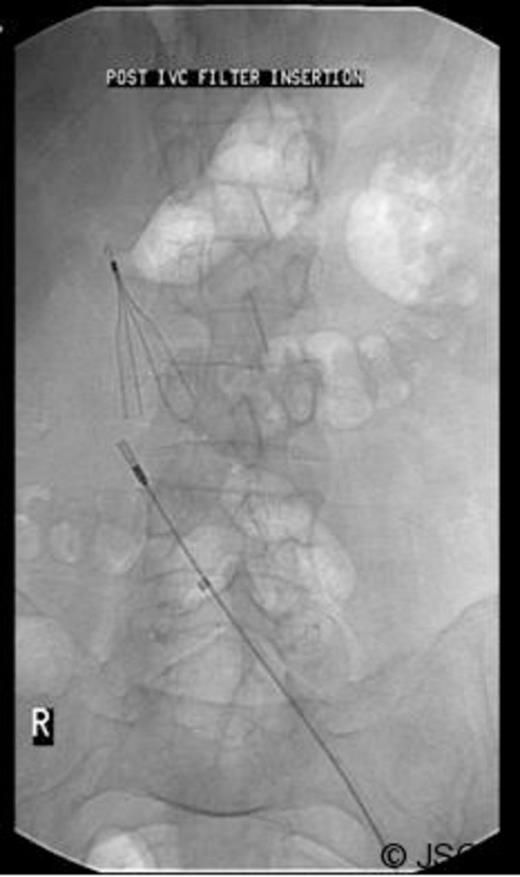
Inferior vena cava (IVC) filter inserted prior to revision surgery
A simultaneous posterior approach to the right hip was used. The total hip replacement was dislocated revealing the acetabular construct deep within the pelvis. The cup was then extracted from the acetabulum under direct vision from the inside of the pelvis with the vascular slings in place. No vascular injury occurred.
The acetabulum was then reconstructed using a Burch Schneider ring with a combination of morsellised and chipped allograft impacted into the medial wall. A 46mm acetabular cup was cemented into the Burch Schneider ring. By the end of the procedure, the normal hip centre of rotation was restored, the leg lengths were equal and the hip was stable.
He was admitted to the High Dependency Unit for post operative recovery where he spent 6 days. On return to the elective ward, he made an uneventful recovery and required anticoagulation with warfarin for six months to protect the IVC filter. The most recent radiograph of his pelvis (Figure 4) showed excellent incorporation of the bone graft.

Regular out-patient reviews at 6 weeks, 3 months and 12 months reported satisfactory progress. Progression from crutches to independent mobilisation occurred during this time period.
DISCUSSION
Protrusio acetabuli is medial displacement of the acetabulum beyond the radiographic teardrop with medial migration of the femoral head into the pelvis (1). Acetabular protrusion may be found in many bone disorders such as degenerative joint disease, Paget's disease, rheumatoid arthritis, ankylosing spondylitis, osteomalacia, Marfan's disease and as an effect of irradiation (2,3).
Diagnosis of protrusio acetabuli is made on the basis of an antero-posterior radiograph of the pelvis that demonstrates a centre-edge angle greater than 40 degrees and medialization of the medial wall of the acetabulum past the ilioischial line(4).
Care must be taken to avoid intra-pelvic intrusion of hardware or cement during acetabular reconstruction to avoid immediate and late injury to the iliac vessels.
Vascular injuries associated with hip arthroplasty consist of thromboembolic complications leading to distal ischaemia, vessel lacerations, pseudo aneurysms, and arterio-venous fistulas (5). Complications are related to cement incorporation of the iliac vessels, aggressive medial retraction, excessive traction on atherosclerotic vessels, and improper technique in preparation of the acetabulum (6).
Risk factors for vascular injuries associated with total hip arthroplasty include revision procedures, left-sided procedures and intra-pelvic migration of the acetabular component of the hip prosthesis (6).
Revision arthroplasty of the hip joint using acetabular reinforcement rings yields good results with the primary assignment being the fixation of the ring to the vital bone.
Acetabular reinforcement rings include Muller rings, Ganz rings, Burch-Schneider rings, and individual acetabular implants.
Reconstruction of acetabular bone stock loss with autologous morcellised bone grafts is an attractive technique with good results.
In patients at risk of vascular injury after primary hip arthroplasty a protocol that combines a retroperitoneal approach to the iliac vessels with a revision total hip arthroplasty has been described (7).
A two-stage operative approach to intrapelvic migration of total hip prostheses has also been described (8).
In conclusion, this case reports highlights a number of learning points from complications arising from a total hip replacement in patients with protrusio acetabuli. Protrusio acetabuli and its potential complications should be recognised pre-operatively and this surgery should be regarded as a complex primary hip arthroplasty ideally performed by an experienced hip surgeon. Care should be taken not to over-ream the medial acetabular wall. In cases where acetabular meshes are used, the surgical team should have a high index of suspicion for any vascular injury. Finally the learning points in avoiding thromboembolic complications in a similar situation are to insert a cava filter, to approach from both sides of the ileum to have access to the external iliac vessels and to undertake a revision total hip arthroplasty.



