-
PDF
- Split View
-
Views
-
Cite
Cite
Vikal Chandra Shakya, Chandra Shekhar Agrawal, Sudeep Khaniya, Gunraj Paudel, Kajan Raj Shrestha, Shailesh Adhikary, Transhepatic perforation of the gallbladder: rare complication of a common disease, Journal of Surgical Case Reports, Volume 2010, Issue 3, May 2010, Page 4, https://doi.org/10.1093/jscr/2010.3.4
Close - Share Icon Share
Abstract
Acute cholecystitis leading to gallbladder perforation is relatively common. However, transhepatic perforation of the gallbladder leading to biliary peritonitis is very rare. We present a rare case of biliary peritonitis caused by transhepatic perforation of the gallbladder.
INTRODUCTION
Gallbladder perforation is one of the most severe and life-threatening complications of acute cholecystitis.(1,2) However, transhepatic perforation of the gallbladder is relatively rare, with less than 20 cases reported in the literature.(3–5) We present a 60 year old male person who presented with this rare condition.
CASE REPORT
A 60 year-old man presented to the emergency department with history of generalized abdominal pain for 5 days starting from the epigastric region, vomiting and not passing stool and flatus. He used to have previous pain in the epigastric region, which used to relieve on taking analgesics and antacids. On examination, he was dehydrated, had tachycardia and hypotension and mild jaundice. Abdominal examination revealed a distended abdomen with generalized tenderness, rebound tenderness and rigidity. His hemoglobin was 10.3gm, total leucocyte count 16358/mm3, with 78% of neutrophils, total bilirubin 3.4mg/dl, conjugated bilirubin 1.5mg/dl, alanine aminotransferase 152 u/li, aspartate aminotransferase 207 u/li, and alkaline phosphatase 386 u/li. An erect abdominal radiograph showed ground glass appearance without free gas under the diaphragm. An ultrasonography of the abdomen showed thick walled, distended gallbladder with multiple gallstones and free fluid all over the peritoneal cavity.
A provisional diagnosis of peritonitis was made and after resuscitation an emergency laparotomy was performed. In the peritoneal cavity there was 2 litres of bilious fluid along with multiple small gallstones free in the peritoneal cavity. Further examination revealed an acutely inflamed thick-walled gallbladder that had perforated through the hepatic parenchyma (Figure 1).
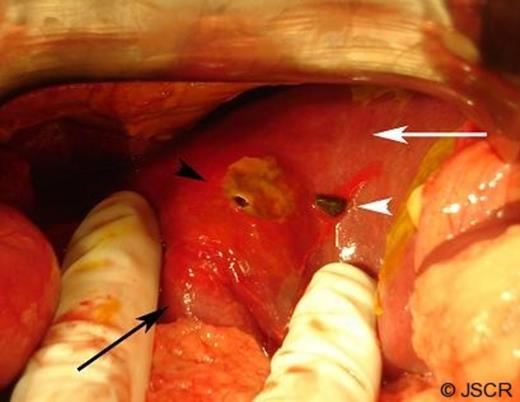
Laparotomy showing the inflamed gallbladder (black arrow), the liver (white arrow), perforation in the liver (black arrowhead), and a gallstone lying adjacent to the perforation (white arrowhead).
A thorough peritoneal lavage was done, cholecystectomy was performed, minute biliary radicals and bleeders were looked for in the exposed liver parenchyma, which were not found. The gallbladder specimen showed the perforation in the fundus (Figure 2).

The excised gallbladder specimen showing the perforation (black arrow) and the cystic duct opening (white arrow).
The histopathology was suggestive of acute cholecystitis with areas of necrosis around the perforation. The patient had an uneventful postoperative recovery.
DISCUSSION
Gallbladder perforation was first reported by Duncan in 1889.(3,6) Rates of gallbladder perforation have been reported to be 2–11% of acute cholecystists.(2,6,7) Nimeier et al divided gallbladder perforation into chronic perforation (type 1), subacute perforation (type 2), and acute free perforation (type 3), which is the most common.(8) Important risk factors for gallbladder perforation are old age (over the age of 60), male gender, previous attacks of cholecystitis, other severe systemic diseases (malignancy, diabetes mellitus, coronary arterial diseases, renal diseases, diabetes mellitus, collagen vascular diseases, obesity, arteriosclerosis, immunosuppression and long-term use of steroids).(3,4,9) In acute cholecystitis, perforation occurs due to inflammation developing into ischemia and necrosis. It occurs most frequently in the fundus because this is the distal most portion and least vascularized region of the gallbladder – ischemia probably plays a crucial role in the pathogenesis of gallbladder perforation. (2,3,7)
In the present case, due to an unstable preoperative condition and generalized peritonitis, further radiological examinations were not performed, and straightaway, an exploratory laparotomy was done. Further radiological investigations such as computed tomography (CT) scan would have increased the possibility of increasing the preoperative diagnosis. A case presenting with localized peritonitis may be very difficult to differentiate from acute cholecystitis. In such stable patients, these investigations definitely have a role before embarking upon the decision of laparotomy. Though a perforation of the gallbladder was not picked up, defect in the wall of the gallbladder in radiological investigations is a reliable evidence for perforation. The radiological determination of the defect on the lining of the wall is hence very important for diagnosis.(5) With high resolution US devices, such defects can be observed in 70% of all perforations. However, US has been found to have low sensitivity for detecting perforations.(1) CT scan can detect the intraperitoneal free fluid, pericholecystic free fluid, abscess, thickening of the wall in the gallbladder, and the defect on the wall which are highly suggestive of gallbladder perforation.
Gallbladder perforation have usually been found to be due to acute calculous cholecystitis.(7) Transhepatic rupture of the gall bladder has been found to result in a hemoperitoneum.(3–5) The present case is unique in the presentation of peritonitis rather than hemoperitoneum. The treatment of choice for transhepatic perforation of the gallbladder is cholecystectomy with debridement of the liver parenchyma and ligation of any biliary radicals and vessels encountered. Though rare, gallbladder perforation should always be considered in the differential diagnosis of peritonitis, especially in elderly patients with findings of cholelithiasis.



