-
PDF
- Split View
-
Views
-
Cite
Cite
A Tandon, MN Abdul Karim, A Muddaiah, P Baranyovits, A case report of chronic frontal bone osteitis presenting with recurrent unilateral lid swelling, Journal of Surgical Case Reports, Volume 2010, Issue 10, December 2010, Page 1, https://doi.org/10.1093/jscr/2010.10.1
Close - Share Icon Share
Abstract
Despite the advances in modern antimicrobial treatment, paranasal sinus disease remains relatively common. A case of chronic inflammatory frontal sinus disease presented with unilateral recurrent eyelid swelling. Clinical features and management in conjunction with ENT are discussed. An extensive literature search has shown only one other similar case reported in Russian language whose management details however are not available.
INTRODUCTION
Orbital complications of para nasal sinusitis such as acute periorbital cellulitis, are well known. (1,2) In the absence of classic symptoms, however the diagnosis may be delayed and result in chronicity. We present a case where the underlying sinus pathology was brought to attention only following a trivial trauma to the eyelid.
CASE REPORT
A 49 year old male gardener presented to the eye clinic with a 3 month history of recurrent painful swelling of the right upper eyelid. The episodes occurred every 2-3 weeks with spontaneous resolution every time. He linked the problem to an injury 3 months previously from a sharp twig while pruning a coniferous tree. His vision had never been affected until the present episode when an enormously swollen upper lid caused total ptosis obscuring the visual axis.
On examination, his vision in the affected right eye was 6/36 and 6/4 in the left. He had complete ptosis with a firm and mildly tender swelling of the right upper lid with no palpable mass lesion or bruit (Figure 1). Extra ocular movements were full. His conjunctiva was injected but not chemosed. His left eye examination was normal.

Suspecting a possible retained orbital foreign body, an urgent CT scan was requested. It showed a bony defect in the right superior orbital rim secondary to chronic frontal bone osteitis and chronic inflammatory sinusitis involving frontal and maxillary sinuses bilaterally (Figure 2). Right globe was normal with normal extra ocular muscles, optic nerve and superior ophthalmic vein. In addition, massive thickening of pre septal soft tissues of the right orbit was noticed with no evidence of any retained foreign body.
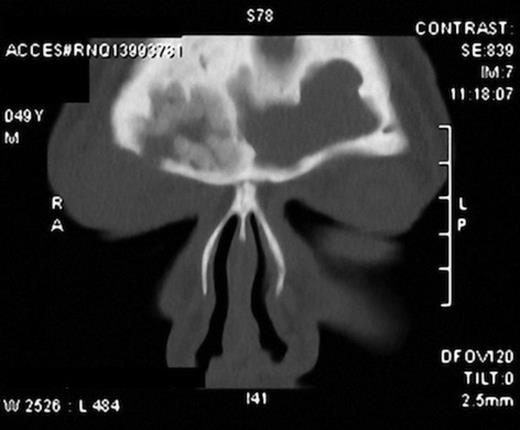
CT scan showing defect in the right superior orbital rim and periorbital soft tissue swelling. Also seen are the inflamed sinus cavities.
With a concurrent course of systemic antibiotics, patient was referred to ENT colleagues for excision of the necrotic frontal bone. A bitemporal coronal incision was made just behind the hair line to give a wide access. The scalp flap was pulled caudally till the supraorbital ridge revealing the periosteum which was then incised. Necrotic bone was removed and the osteotomy was then enlarged. The mucosal lining was peeled off under the microscopic view to ensure a complete removal. Fascia lata harvested from the thigh was then used to obliterate both the frontal sinus cavities. Nasal endoscopy also showed ethmoidal sinus congestion for which topical betnesol drops were prescribed for 6 weeks. Just 2 weeks post operatively, lid swelling disappeared completely with restoration of vision to 6/6 and normal anterior segment.
Histology of the excised bone confirmed inflammatory osteitis with no evidence of infective osteomyelitis.
DISCUSSION
Periorbital cellulitis secondary to sinusitis is a common clinical entity. In appropriate clinical settings, such as sickle cell disease and immune deficiency disorders, infective organisms varying from Salmonella to Mycobacterium tuberculosis and Trepanoma pallidum can cause acute or chronic inflammation. (3,4)
Our patient had recurrent unilateral lid swelling as a complication of chronic frontal sinusitis causing bony osteitis. (5,6) The history suggestive of a possible retained foreign body was in all probability a coincidence but contributed to delay in patient’s presentation. However, previous nasal polypectomy could have also contributed to chronicity of sinusitis. (7) An extensive search of the literature has shown only one case reported in Russian literature with similar findings but the details of the management are not available. (8) Our patient was unusual in his presentation with symptoms solely confined to one eye with a firm, recurrent swelling of the upper lid. A radical removal of the necrotic bone along with obliteration of sinus cavities proved curative. (9)



