-
PDF
- Split View
-
Views
-
Cite
Cite
Ahmed Alanzi, Bano Alsaleh, Dawood Alatefi, Khaled M AlAani, Hosameldin Mohamad, Recurrent renal hydatid disease with suspected pelvic seeding: a case report, Journal of Surgical Case Reports, Volume 2026, Issue 1, January 2026, rjaf735, https://doi.org/10.1093/jscr/rjaf735
Close - Share Icon Share
Abstract
Renal hydatid disease is a rare manifestation of echinococcosis, accounting for ˂4% of cases. We report a 47-year-old male with two prior surgeries for right renal hydatid cysts, presenting with right upper quadrant pain, dysuria, and low-grade fever. Imaging revealed a recurrent right renal cystic lesion and an incidental pelvic cyst near the seminal vesicle, raising concern for possible dissemination. Laparoscopic aspiration and deroofing of the renal cyst were performed, followed by a 6-month course of albendazole. Recovery was uneventful, and follow-up imaging showed no recurrence or new cyst formation. This case highlights the importance of long-term surveillance in renal hydatid disease and the need to consider rare sites of recurrence or dissemination. Multimodal imaging and minimally invasive surgery play a central role in diagnosis and management, even in patients outside endemic regions.
Introduction
Echinococcosis is a parasitic zoonosis caused by Echinococcus granulosus, primarily endemic to the Middle East, Mediterranean region, South America, and parts of Asia and Africa [1]. Humans contract the infection via ingestion of parasitic eggs through contaminated food, water, or contact with infected dogs. The liver and lungs are the most commonly involved organs, but kidneys may also be affected in ⁓2%–4% of cases [2]. Renal hydatid cysts may remain asymptomatic for years due to their slow growth, and when symptomatic, may present with flank pain, hematuria, or hydatiduria. Diagnosis relies on imaging, particularly ultrasound and computed tomography (CT), supported by serology when available [3]. Treatment involves surgery with or without antiparasitic therapy, and recurrence can occur despite adequate management [4].
Case presentation
A 47-year-old male presented with a 3-week history of right upper quadrant pain, nausea, vomiting, dysuria, low-grade fever, and reduced appetite. He denied weight loss, rectal bleeding, or recent travel to endemic areas. He had undergone laparoscopic deroofing of a right renal hydatid cyst in 2014 and again in 2022.
On examination, he was hemodynamically stable. Abdominal exam revealed right flank tenderness and a palpable mass. Laboratory investigations, including complete blood count, liver and renal function tests, and echinococcal serology, were within normal limits. Urinalysis and urine culture were negative.
Ultrasound showed a large cystic lesion in the right kidney with internal debris and fluid–fluid levels (Fig. 1). Contrast-enhanced CT confirmed a thick-walled, fluid-filled cyst in the right upper renal pole without septations or calcifications—consistent with recurrent hydatid disease (Fig. 2). Incidentally, a small pelvic cystic lesion was seen adjacent to the rectum and seminal vesicle.
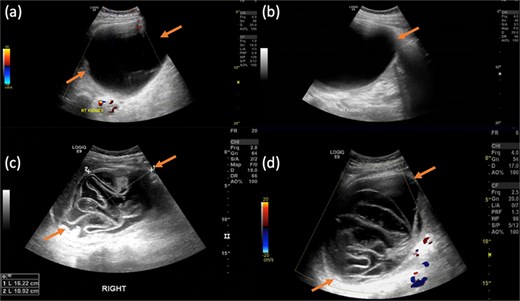
Gray-scale transabdominal ultrasound demonstrates a large well-defined anechoic lesion located in the upper pole of the kidney. The lesion contains internal, non-septated debris and shows no internal vascularity on color doppler imaging (a and b). Compared with previous right renal lesion showing collapsed membranes float within the cyst fluid, resembling water lily.
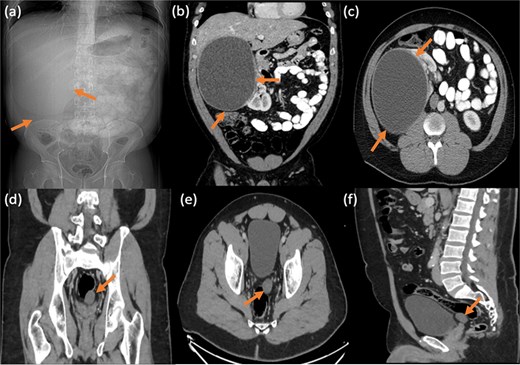
Frontal abdominal radiograph in supine position showing opacity occupying the right upper abdominal region with paucity of bowel loops (a). Followed by contrast enhanced CT abdomen and pelvis with reconstructed images showing a large thick walled non-septated non-calcific right renal cortical cyst (b and c). No right perinephric/pericystic fat stranding or free fluid, preserved tissue planes with surrounding related organs. Incidentally noted small similar looking cystic lesion in the left pelvic region, inseparable from the rectal wall and left seminal vesicle showing no gross fat or calcification (d–f).
Pelvic magnetic resonance imaging (MRI) further characterized the pelvic lesion as a well-defined, non-enhancing, fluid-filled cyst measuring 3 × 2 × 1 cm without solid components, raising suspicion for pelvic hydatid seeding, although peritoneal inclusion cyst was also considered (Fig. 3). A 99mTc-dimercaptosuccinic acid (DMSA) scan showed preserved renal function with the right kidney contributing 25.7% of total function and a photopenic defect at the cyst site (Fig. 4). No other lesions were found on chest CT or brain MRI. Colonoscopy ruled out malignancy but revealed incidental low-grade adenomas.
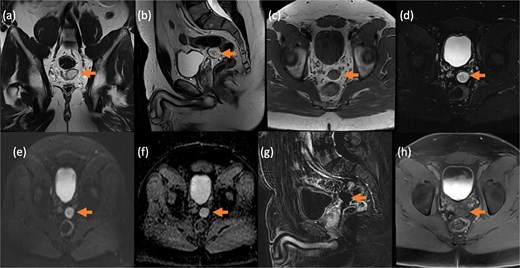
Contrast-enhanced MRI of the pelvis in different sequences and different planes demonstrates a small, well-defined, oval-shaped lesion with high signal intensity on T2-weighted images (bold arrow—a and b) and low signal intensity on T1-weighted images (bold arrow—c). The lesion is located in the pelvis, inseparable from the seminal vesicles and the anterior rectal wall. It shows no signal drop on fat-saturated T2 sequence (bold arrow—d) no signify macroscopic fat, no restricted diffusion (dashed arrow—e and f) with T2 shine through, and no post-contrast enhancement on early subtracted (arrow head—g) and no delayed enhancement (arrow head—h). No solid component.
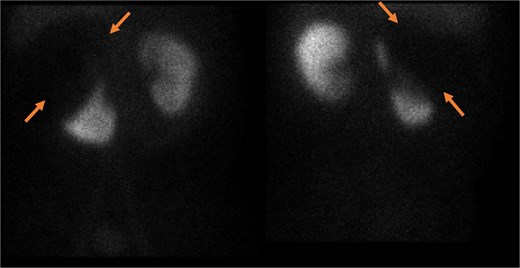
Static image of the abdomen at 2 h after IV injection TC-99 m DMSA, showing normal morphology & corticotubular function of the left kidney. Large photopenic area occupying the upper half of the right kidney while its lower half showed preserved cortical function.
The patient underwent laparoscopic aspiration and deroofing of the renal cyst. Recovery was uneventful. He was started on albendazole 400 mg twice daily for 6 months with monthly liver function monitoring. At 3-month follow-up, he remained asymptomatic, and imaging showed no recurrence. The incidental pelvic cyst remained unchanged in size and appearance and, given its small size, lack of enhancement, and benign imaging features, it was managed conservatively with continued radiological surveillance.
Discussion
Renal hydatid disease presents diagnostic challenges due to its rarity and often non-specific symptoms. In this case, serological tests were negative—a known limitation in isolated renal hydatid disease due to low sensitivity in localized infections [3]. Imaging played a pivotal role in diagnosis and surveillance. CT confirmed cystic recurrence, and MRI was essential in evaluating the pelvic lesion. Although rare, pelvic seeding may result from intraoperative spillage or rupture [2]. In our patient, the pelvic lesion was managed conservatively with serial imaging, as its stability and benign features supported observation rather than intervention.
MRI findings—high T2 signal, absence of enhancement, and lack of diffusion restriction—suggested a benign cyst. Yet, the patient’s surgical history warranted suspicion for secondary hydatid dissemination. This highlights MRI’s value in soft tissue evaluation where CT may be limited [5].
Functional imaging confirmed adequate residual function in the affected kidney, supporting a nephron-sparing surgical approach such as cyst excision or partial nephrectomy. Surgical management remains the cornerstone of treatment for renal hydatid disease, with laparoscopic techniques favored due to reduced morbidity and faster recovery [6, 7]. This minimally invasive approach is particularly advantageous in recurrent cases, where prior surgeries may result in adhesions and distorted anatomy.
Albendazole is the antiparasitic agent of choice. Preoperative therapy may sterilize the cyst, while postoperative treatment reduces recurrence risk by targeting residual or disseminated larvae [8, 9]. Our patient completed a 6-month course with regular liver function monitoring and no adverse effects.
Long-term follow-up is essential, as recurrence may occur years after surgery. This patient had two recurrences across nearly a decade, emphasizing the need for surveillance imaging and clinical monitoring. Although extra-renal dissemination is rare, reports have documented peritoneal, pelvic, and even central nervous system involvement [10].
Conclusion
This case illustrates the recurrent and potentially disseminated nature of renal hydatid disease, the diagnostic limitations of serology, and the value of multimodal imaging. The incidental detection of a pelvic cyst underscores the importance of comprehensive evaluation. Laparoscopic management combined with albendazole therapy yielded a favorable outcome. Lifelong surveillance remains key to early detection of recurrence and prevention of complications.
Conflict of interest statement
The authors declare no conflicts of interest related to this case report.
Funding
No funding was needed for this case report.
Patient consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editorial office upon request.



