-
PDF
- Split View
-
Views
-
Cite
Cite
Tal Weiss, Dror Karni, Veacheslav Zilbermints, Boris Kessel, Oren Gal, Unmasking the false cecal polyp: a case of inverted appendix—a case report and review of the literature, Journal of Surgical Case Reports, Volume 2026, Issue 1, January 2026, rjaf1083, https://doi.org/10.1093/jscr/rjaf1083
Close - Share Icon Share
Abstract
An inverted appendix is a rare incidental finding on colonoscopy, often misinterpreted as a neoplastic lesion. A 74-year-old woman underwent routine screening colonoscopy that revealed a cecal polypoid lesion near the appendiceal orifice. Initial biopsies showed nonspecific inflammation, and a subsequent contrast-enhanced computed tomography (CT) scan reported only sigmoid diverticulosis. During a repeat in-hospital colonoscopy, the lesion was re-evaluated and identified as an inverted appendix, preventing unnecessary resection. Retrospective review of the CT images confirmed the diagnosis. Appendiceal inversion may result from surgical manipulation, intussusception, or rarely congenital causes, and is characterized endoscopically by origin at the appendiceal orifice, normal mucosa, and distinctive imaging features. Rarely, it may be associated with mucinous, neuroendocrine, or endometriotic lesions. Awareness of this entity is vital, as biopsy or removal of benign-appearing lesions is not indicated and may result in bleeding or perforation. Careful endoscopic assessment and imaging review are essential to avoid unnecessary resection.
Introduction
Appendiceal inversion, or appendiceal intussusception, is an uncommon endoscopic finding, with estimated prevalence around 0.01% in surgical and colonoscopic series [1, 2]. Its clinical importance arises from its capacity to mimic polyps or neoplastic lesions of the cecum, which can lead to unnecessary or harmful interventions. While many inverted appendices are benign, there are occasional reports of associated pathology, including endometriosis [3], mucinous neoplasms [4], and neuroendocrine tumors [5]. This case report describes an incidentally discovered inverted appendix, its evaluation, and management, along with a concise review of the literature.
Case presentation
A 74-year-old woman with a significant past medical history, including right mastectomy for breast carcinoma followed by adjuvant radiotherapy and ischemic heart disease, underwent a routine screening colonoscopy in January 2024 in an outpatient setting. Her only prior abdominal surgery was a prophylactic bilateral oophorectomy, and she had no history of appendectomy. Her previous colonoscopies were otherwise unremarkable, with only mild sigmoid diverticulosis noted. The current procedure again demonstrated diverticulosis in the sigmoid colon and a cecal elongated polypoid lesion adjacent to the appendiceal orifice. Biopsies were obtained, and histopathology results were consistent with nonspecific inflammation.
Subsequently, in January 2025, a contrast-enhanced computed tomography (CT) scan was performed for further evaluation of the lesion. The formal outpatient CT report described only sigmoid diverticulosis. The patient was then scheduled for an in-hospital polypectomy. During the repeat colonoscopy performed in May 2025, the same cecal lesion was confirmed, becoming evident after removal of the overlying fecal content. The lesion, originating from the appendiceal orifice, was evaluated by two endoscopists and a surgical consultant. Its structure and mucosal appearance were not suspicious for a polyp but rather consistent with an inverted appendix (Fig. 1).
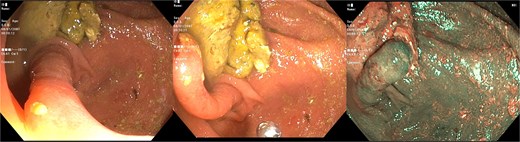
Colonoscopic image of the cecum showing characteristic features consistent with an inverted appendix.
The outpatient abdominal CT images were reviewed, and the diagnosis of an inverted appendix was confirmed (Fig. 2).

Coronal contrast-enhanced CT scan demonstrating an elongated structure projecting into the cecal lumen from the appendiceal orifice, consistent with an inverted appendix.
A multidisciplinary discussion was held, and in light of the above-mentioned characteristics, the decision was made to defer endoscopic resection.
Discussion
The mechanisms of appendiceal inversion include historic iatrogenic inversion techniques employed during open appendectomy, in which the stump was inverted into the cecum and ligated. While this method is now rarely performed, it accounts for a significant proportion of cases described in older surgical series [1]. True intussusception of the appendix is another cause, typically resulting from abnormal peristalsis or the presence of a lead point lesion, and may present with chronic abdominal pain or mimic neoplastic disease [6]. Congenital inversion, although exceedingly rare, has been reported in both children and adults without prior surgery [7]. In large clinicopathologic analyses, inverted appendices were most frequently detected incidentally during colonoscopy performed for unrelated indications, underscoring their often silent nature [1].
While many inverted appendices are benign, they can sometimes harbor significant pathology. Endometriosis has been reported as a rare cause of appendiceal intussusception, sometimes leading to obstructive symptoms or acute appendicitis [3, 8]. Malignant associations include low-grade appendiceal mucinous neoplasms, serrated adenomas, and neuroendocrine tumors [1, 5]. In the largest clinicopathologic series of 21 cases, nearly one-third were associated with underlying pathology such as mucinous neoplasms or adenomas [1]. Importantly, cases of unsuspected appendiceal carcinoma have also been described in the setting of inversion, highlighting the need for careful evaluation [5].
Radiologic imaging plays a central role in confirming the diagnosis and excluding malignancy. CT typically demonstrates a tubular structure invaginating into the cecum, which correlates with the endoscopic impression of a polypoid lesion at the appendiceal orifice [5, 9]. Cross-sectional imaging is particularly useful in distinguishing benign inversion from neoplastic causes, as appendiceal carcinoid tumors may appear as mural thickening with or without enhancement [5]. Positron emission tomography or magnetic resonance imaging may also be used to further characterize lesions when suspicion for malignancy is high [5]. Recognition of these radiologic patterns helps avoid unnecessary intervention while ensuring that pathologic conditions are not overlooked.
The optimal management of an inverted appendix depends on clinical presentation and associated findings. In asymptomatic patients with benign-appearing lesions and supportive radiology, conservative management with observation is appropriate [6]. Biopsy or endoscopic resection of inverted appendices carries a risk of perforation and delayed peritonitis, as demonstrated in reports of complications after polypectomy [1, 10]. Endoscopic techniques such as endoloop-assisted appendectomy have been described for selected cases, particularly when the lesion is symptomatic or neoplastic [11]. Surgical appendectomy or right hemicolectomy remains the treatment of choice when malignancy is confirmed or strongly suspected [4].
This case highlights the importance of thorough endoscopic evaluation combined with careful review of abdominal imaging. Correlation of clinical, endoscopic, and radiologic findings consistent with benign appendiceal inversion allowed avoidance of unnecessary intervention.
Conclusion
An inverted appendix should be included in the differential diagnosis whenever a cecal lesion is identified during colonoscopy, especially at the appendiceal orifice. Characteristic endoscopic and imaging features allow a non-interventional approach in most asymptomatic cases. Intervention should be reserved for suspected neoplasia or symptomatic cases.
Author contributions
Tal Weiss drafted the manuscript, collected the clinical data, and performed the literature review. Boris Kessel and Veacheslav Zilbermints supervised the work and provided critical revisions. Oren Gal performed the index endoscopy and contributed to the manuscript review. Dror Karni also contributed to the review of the manuscript.
Conflict of interest statement
The authors declare no conflicts of interest.
Funding
None declared.
Patient consent for publication
According to the policy of our institution, specific patient consent is not required for publication of a single anonymized case report.



