-
PDF
- Split View
-
Views
-
Cite
Cite
Yuki Etani, Takaaki Noguchi, Makoto Hirao, Tasuku Miyake, Seiji Okada, Ken Nakata, Kosuke Ebina, Combination of midfoot derotational osteotomy and ankle arthrodesis against neglected clubfoot: a case report, Journal of Surgical Case Reports, Volume 2026, Issue 1, January 2026, rjaf1079, https://doi.org/10.1093/jscr/rjaf1079
Close - Share Icon Share
Abstract
Neglected congenital clubfoot in adults is difficult to manage. Multi-joint arthrodesis is often required but is invasive and associated with complications. We report an adult case treated with ankle arthrodesis and midfoot derotational osteotomy. A 59-year-old man with untreated idiopathic clubfoot since birth presented with severe hindfoot varus and rigid midfoot inversion, leading to wheelchair dependence. Imaging showed correctable hindfoot deformities but rigid midfoot inversion with talonavicular subluxation. Surgery consisted of Achilles tendon lengthening, ankle and subtalar arthrodesis with a retrograde intramedullary nail, and midfoot derotational osteotomy, resulting plantigrade. Bony union was confirmed at one year. At 3 years, plantigrade alignment remained without recurrence. Callosities resolved, and the patient regained pain-free walking. Clinical scores improved: Japanese Society for Surgery of the Foot ankle/hindfoot (4.0 to 66.0), Japanese Society for Surgery of the Foot midfoot (0.0 to 73.0), self-administered foot evaluation questionnaire (89.2 to 366.0). This is the first report of midfoot derotational osteotomy for neglected congenital clubfoot, offering a less invasive option for selected adults.
Introduction
Congenital clubfoot is a common pediatric deformity that can usually be corrected effectively in infancy using the Ponseti method [1–4]. When untreated, however, it may persist into adulthood as “neglected clubfoot,” which is difficult to manage due to rigidity and contractures [4].
Various surgical strategies have been reported, ranging from soft tissue procedures and osteotomies to multi-joint arthrodesis and external fixation [5–8]. In severe cases, multi-joint arthrodesis is often required, but this procedure is invasive and carries risks including nonunion and stiffness. Thus, there is no consensus on the optimal treatment, and individualized approaches are required.
Midfoot derotational osteotomy [9, 10] has been described for severe deformities in rheumatoid arthritis, trauma, or poliomyelitis, but, to our knowledge, has not been reported for neglected congenital clubfoot. We present a 59-year-old man with adult neglected clubfoot successfully treated by combining ankle arthrodesis with midfoot derotational osteotomy.
Case report
A 59-year-old man had exhibited a right clubfoot deformity since birth. At infancy, he was thoroughly examined by a pediatrician and an orthopedic surgeon, who excluded neuromuscular disorders and diagnosed idiopathic congenital clubfoot. Although surgical treatment was recommended, he did not undergo correction because of financial constraints. Despite the persistent deformity, he was able to walk during childhood and adulthood, and therefore did not seek further medical attention.
Two years before presentation, his deformity worsened and pain increased, resulting in progressive walking difficulty and wheelchair dependence. Physical examination revealed severe varus and equinus deformity of the ankle with painful callosities on the lateral midfoot (Fig. 1A and B). The range of motion of the ankle was markedly restricted, with −45° dorsiflexion and 60° plantarflexion.

Preoperative photographs of the right foot. (A) The ankle joint showed varus and equinus deformity. (B) Painful callosities on the lateral aspect of the foot.
Preoperative radiographs demonstrated marked varus deformity of the ankle and abnormal weight-bearing on the lateral border of the foot (Fig. 2A and B). Under valgus stress, correction of the ankle and subtalar deformities was possible, but the midfoot inversion remained uncorrectable (Fig. 2C). Computed tomography revealed midfoot inversion associated with talonavicular subluxation (Fig. 3A and B). Based on these findings, surgical treatment aimed at achieving a plantigrade foot and restoring ambulation was planned.
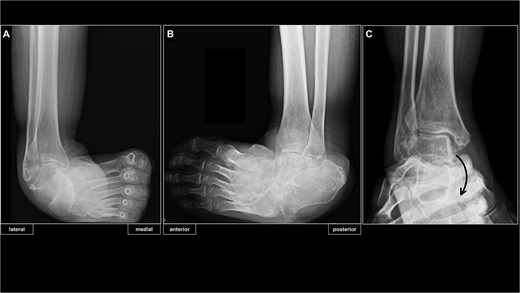
Preoperative radiographs of the right ankle. (A) Radiograph of right ankle in the antero-posterior weight-bearing view. (B) Radiograph of right ankle in the latero-medial weight-bearing view. (C) Preoperative ankle stressed imaging showed correctability of ankle and subtalar joint deformities, but non-correctable subluxation of the talonavicular joint.
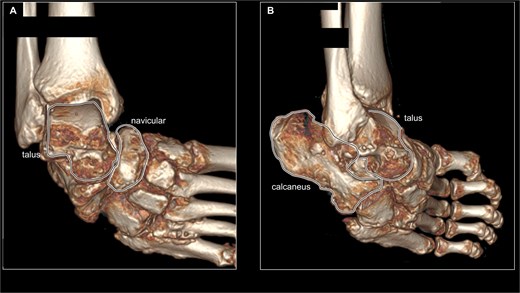
Preoperative CT imaging of the right foot. (A) 3D reconstructed image of preoperative CT scan from ankle joint frontal view. The talus and navicular bones are surrounded by black lines, showing subluxation of the talonavicular joint. (B) 3D reconstructed image of preoperative CT scan from ankle joint anterolateral view. The talus and calcaneus are surrounded by a black line, showing marked varus deformity of the subtalar joint.
The surgery was performed in three steps. First, after removal of osteophytes and decortication of the joint surfaces as part of joint preparation for arthrodesis, Achilles tendon lengthening with gastrocnemius recession [11] was performed, allowing correction of the ankle to neutral dorsiflexion. Second, ankle and subtalar arthrodesis was achieved using a retrograde intramedullary nail (Ankle Phoenix Nail®, Zimmer Biomet, Warsaw, IN, USA) through a lateral approach. Although hindfoot correction was obtained, the rigid midfoot inversion persisted. Third, a midfoot derotational osteotomy was performed from the first cuneiform to the cuboid, dividing the bone into proximal and distal segments (Fig. 4A and B). The midfoot was manually derotated to correct the inversion, achieving plantigrade. Then, the osteotomy site was fixed with percutaneous 2.0-mm Kirschner wires inserted from distal to proximal (Fig. 4C–E), while carefully avoiding injury to the dorsalis pedis artery.
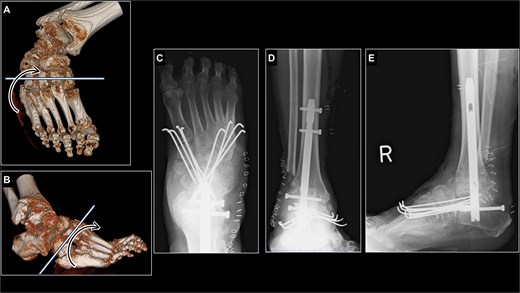
Surgical planning and postoperative radiographs of the right foot just after surgery. (A, B) an osteotomy line was established from the first cuneiform to the cuboid. (C) Midfoot derotational osteotomy site was fixed with eight K-wires. (D, E) Hindfoot was fixed with retrograde intramedullary nail while varus and equinus deformity was corrected.
Postoperatively, the ankle was immobilized with a cast and non–weight bearing was maintained for 5 weeks. After removal of the cast and Kirschner wires, partial weight bearing with an ankle orthosis and gait training were initiated. Full weight bearing was permitted 8 weeks after surgery. Three months postoperatively, the patient achieved stable walking with a walker and was discharged. At 1 year postoperatively, radiographs confirmed union at the osteotomy site and maintained correction of the varus deformity (Fig. 5A and B). The painful callosities had resolved (Fig. 5C and D). Functionally, the patient was able to walk without pain using a walker for outdoor ambulation. At 3 years postoperatively, the patient has remained free from recurrence of the deformity, and the clinical scores have improved markedly (Table 1). The JSSF ankle/hindfoot score improved from 4.0 to 66.0, the JSSF midfoot score from 0.0 to 73.0, and the self-administered foot evaluation questionnaire (SAFE-Q) total score from 89.2 to 366.0 [12, 13].

Postoperative radiographs and photographs of the right foot 1 year after surgery. (A, B) radiograph of right ankle in a weight-bearing position showed the fusion of osteotomy site and sustained plantigrade alignment. (C, D) The callosities of lateral aspect of foot had almost come off.
Changes in the Japanese Society for Surgery of the Foot (JSSF) and self-administered foot evaluation questionnaire (SAFE-Q) scores
| Preoperative . | Postoperative (3 years after surgery) . | |
|---|---|---|
| JSSF ankle/hindfoot score | ||
| Pain (40 points) | 0.0 | 30.0 |
| Function (45 points) | 4.0 | 31.0 |
| Alignment (15 points) | 0.0 | 5.0 |
| Total (100 points) | 4.0 | 66.0 |
| JSSF midfoot score | ||
| Pain (40 points) | 0.0 | 30.0 |
| Function (45 points) | 0.0 | 35.0 |
| Alignment (15 points) | 0.0 | 8.0 |
| Total (100 points) | 0.0 | 73.0 |
| SAFE-Q score | ||
| Pain and pain-related (100) | 43.6 | 93.2 |
| Physical functioning and daily living (100) | 2.3 | 63.6 |
| Social functioning (100) | 0.0 | 62.5 |
| General health and well-being (100) | 10.0 | 80.0 |
| Shoe-related (100) | 33.3 | 66.7 |
| Total (500) | 89.2 | 366.0 |
| Preoperative . | Postoperative (3 years after surgery) . | |
|---|---|---|
| JSSF ankle/hindfoot score | ||
| Pain (40 points) | 0.0 | 30.0 |
| Function (45 points) | 4.0 | 31.0 |
| Alignment (15 points) | 0.0 | 5.0 |
| Total (100 points) | 4.0 | 66.0 |
| JSSF midfoot score | ||
| Pain (40 points) | 0.0 | 30.0 |
| Function (45 points) | 0.0 | 35.0 |
| Alignment (15 points) | 0.0 | 8.0 |
| Total (100 points) | 0.0 | 73.0 |
| SAFE-Q score | ||
| Pain and pain-related (100) | 43.6 | 93.2 |
| Physical functioning and daily living (100) | 2.3 | 63.6 |
| Social functioning (100) | 0.0 | 62.5 |
| General health and well-being (100) | 10.0 | 80.0 |
| Shoe-related (100) | 33.3 | 66.7 |
| Total (500) | 89.2 | 366.0 |
Changes in the Japanese Society for Surgery of the Foot (JSSF) and self-administered foot evaluation questionnaire (SAFE-Q) scores
| Preoperative . | Postoperative (3 years after surgery) . | |
|---|---|---|
| JSSF ankle/hindfoot score | ||
| Pain (40 points) | 0.0 | 30.0 |
| Function (45 points) | 4.0 | 31.0 |
| Alignment (15 points) | 0.0 | 5.0 |
| Total (100 points) | 4.0 | 66.0 |
| JSSF midfoot score | ||
| Pain (40 points) | 0.0 | 30.0 |
| Function (45 points) | 0.0 | 35.0 |
| Alignment (15 points) | 0.0 | 8.0 |
| Total (100 points) | 0.0 | 73.0 |
| SAFE-Q score | ||
| Pain and pain-related (100) | 43.6 | 93.2 |
| Physical functioning and daily living (100) | 2.3 | 63.6 |
| Social functioning (100) | 0.0 | 62.5 |
| General health and well-being (100) | 10.0 | 80.0 |
| Shoe-related (100) | 33.3 | 66.7 |
| Total (500) | 89.2 | 366.0 |
| Preoperative . | Postoperative (3 years after surgery) . | |
|---|---|---|
| JSSF ankle/hindfoot score | ||
| Pain (40 points) | 0.0 | 30.0 |
| Function (45 points) | 4.0 | 31.0 |
| Alignment (15 points) | 0.0 | 5.0 |
| Total (100 points) | 4.0 | 66.0 |
| JSSF midfoot score | ||
| Pain (40 points) | 0.0 | 30.0 |
| Function (45 points) | 0.0 | 35.0 |
| Alignment (15 points) | 0.0 | 8.0 |
| Total (100 points) | 0.0 | 73.0 |
| SAFE-Q score | ||
| Pain and pain-related (100) | 43.6 | 93.2 |
| Physical functioning and daily living (100) | 2.3 | 63.6 |
| Social functioning (100) | 0.0 | 62.5 |
| General health and well-being (100) | 10.0 | 80.0 |
| Shoe-related (100) | 33.3 | 66.7 |
| Total (500) | 89.2 | 366.0 |
Discussion
There is no standardized surgical treatment for neglected clubfoot in adults because the pattern and severity of deformities vary considerably among patients [5]. Appropriate correction requires a thorough preoperative assessment of the underlying pathology and careful selection of surgical procedures. In general, soft tissue procedures such as Achilles tendon lengthening and joint capsular release are used to balance contractures, whereas osteotomies, arthrodesis, and Ilizarov external fixation have been employed for bony deformities [5–8]. Among these, multi-joint arthrodesis, including tibiotalar, subtalar, talonavicular, and calcaneocuboid fusions, has often been considered in severe cases [8]. However, this procedure is technically demanding, invasive, and results in loss of Chopart joint mobility.
In the present case, ankle and subtalar arthrodesis corrected the hindfoot deformity but failed to address the rigid midfoot inversion. Rather than proceeding with four-joint fusion at the Chopart joint, which would have been highly invasive, we selected a midfoot derotational osteotomy as a less invasive alternative. This procedure successfully achieved a plantigrade foot and restored pain-free walking ability. Although midfoot derotational osteotomy has been reported in the context of traumatic deformities, rheumatoid arthritis, and poliomyelitis, to the best of our knowledge, its application in neglected congenital clubfoot has not been previously described. This procedure can correct rotational deformities of ~30°, highlighting its role as a feasible option for adult patients with severe midfoot inversion. In neglected clubfoot, persistent lateral midfoot loading contributes to the progression and rigidity of the midfoot varus deformity, indicating that derotational osteotomy may represent an effective corrective strategy. The clinical implication of this case is that midfoot derotational osteotomy can expand the surgical armamentarium for neglected clubfoot, offering a technically less demanding approach compared with multi-joint arthrodesis. Importantly, the achievement of a plantigrade foot should be prioritized, as it enables functional ambulation and improves quality of life [14]. In this patient, postoperative outcomes measured by JSSF and SAFE-Q demonstrated marked improvements in pain, function, and social participation, supporting its functional benefit.
This report is limited by its single-case design and relatively short follow-up. Future studies with larger cohorts and longer observation periods are needed to clarify the durability, recurrence risk, and long-term safety of this technique in adult neglected clubfoot.
Acknowledgements
We would like to thank all the physical therapists, medical assistants, and staff at Osaka University Hospital for their excellent therapy and support.
Conflict of interest statement
None declared.
Funding
None declared.
Patient consent
The patient provided informed consent for this publication prior to inclusion in the report.



