-
PDF
- Split View
-
Views
-
Cite
Cite
Emad Aljohani, De Garengeot hernia presenting with acute appendicitis: a rare dual pathology and surgical challenge: a case report, Journal of Surgical Case Reports, Volume 2026, Issue 1, January 2026, rjaf1073, https://doi.org/10.1093/jscr/rjaf1073
Close - Share Icon Share
Abstract
De Garengeot hernia is uncommon, contributing to ~0.5%–5% of all femoral hernias. A healthy 31-year-old male patient presented with a 3-day history of migrating right lower quadrant pain, nausea, and vomiting. Acute appendicitis was identified on a computed tomography scan. On the Diagnostic laparoscopy, the appendix was extremely inflamed and herniated in the femoral canal, a diagnostic feature of a De Garengeot hernia. The appendix was reduced gently; however, the hernia was not repaired in this index surgery. The patient had an uneventful recovery and was discharged on the first postoperative day. An elective laparoscopic femoral hernia repair was scheduled. De Garengeot hernia with complicated acute appendicitis is an operative and diagnostic challenge. This case is unique due to the patient’s young age. Accurate early diagnosis and an individualized operative plan were key factors in achieving an excellent outcome.
Introduction
The De Garengeot hernia, herniation of the vermiform appendix into the femoral canal, is a rare condition [1, 2]. It is reported largely in the form of case reports and case series, most often as an intraoperative rather than preoperative diagnosis [3, 4]. Femoral hernias represent a minority of all groin hernias, commonly found in women with wide variations globally [4]. The presence of the appendix in the femoral sac is rare, occurring in 0.5%–5% of femoral hernias [5]. Acute appendicitis within that sac is even rarer, with an incidence of 0.08%–0.13% [6, 7]. This pathology in combination is one of the rarest surgical emergencies.
The De Garengeot hernia clinically manifests as an incarcerated femoral hernia [3, 6], with a tender, irreducible groin mass, occasionally with bowel obstruction [6]. The classical findings of acute appendicitis, fever, leukocytosis, or peritonitis, may be absent or mild since the inflamed appendix is walled off within the femoral canal. Thus, preoperative diagnosis is challenging, and most cases are diagnosed only during surgery.
Ultrasound can demonstrate a non-compressible tubular structure within the femoral canal, which can be confirmed by a computed tomography (CT) scan [8]. However, because of the urgency, a definitive diagnosis is still made intraoperatively. Appendectomy with simultaneous hernia repair is the main treatment [9]. Due to the rarity of this condition, there are no guidelines, and advice is drawn mainly from single case reports.
Most reported cases are elderly females [3, 4] and young male incidence is extremely uncommon. We present a rare case of acute appendicitis in a De Garengeot hernia in a young male. This case is noteworthy because it goes against the classical demographic anticipation and illustrates the diagnostic conundrum as well as the surgical challenge in managing this rare condition.
Case report
Case presentation
A 31-year-old male presented to the emergency department with a history of abdominal pain for 3 days. The pain was diffused around the umbilicus, subsequently migrated to the right lower quadrant and to the right groin, and was associated with nausea, vomiting, and anorexia. Abdominal exam revealed severe right lower quadrant and right groin tenderness with rebound tenderness. Laboratory findings showed leukocytosis with a white blood cell count of 17 × 109/L. Contrast-enhanced CT scan of the abdomen and pelvis revealed findings consistent with acute, uncomplicated appendicitis, including an appendix ~1 cm in diameter and periappendiceal fat stranding. The appendix was visualized to be within the pelvis (Fig. 1).

CT scan of the abdomen and pelvis showing acute appendicitis with the appendix extending toward the right femoral canal.
Surgical technique
The patient was scheduled for a diagnostic laparoscopy, which revealed an inflamed appendix herniated inside the femoral canal, consistent with a De Garengeot hernia (Fig. 2). The appendix was brought down cautiously from the femoral canal. Laparoscopic appendectomy was subsequently carried out, and hemostasis was obtained. The appendix base was tied, and then was removed in a sterile bag. Hernioplasty was not performed in the index procedure to avoid potential mesh infection.
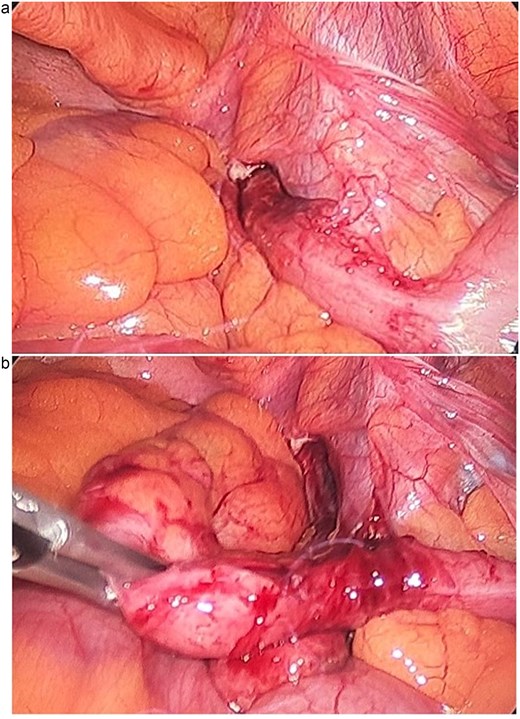
Intraoperative laparoscopic views. (a) Inflamed appendix herniated within the femoral canal, consistent with a De Garengeot hernia. (b) The appendix following reduction from the femoral canal prior to appendectomy.
Postoperative course
The postoperative course was uneventful, and the patient was discharged in good condition. He was counseled regarding the intraoperative findings at the follow-up visit and gave elective consent for laparoscopic femoral hernia repair.
Discussion
Acute appendicitis complicating De Garengeot hernia is a rare clinical entity that intrigue surgeons due to its diagnostic enigma and therapeutic dilemma. In our patient, the atypical presentation in a young male further adds to its value, as most reported cases are in older females [10, 11]. This aberrant demographic highlights the importance of still maintaining a broad differential diagnosis when evaluating patients with groin masses, regardless of age or sex.
Preoperative diagnosis of a De Garengeot hernia is very difficult to make. Clinical presentation is typically nonspecific, consisting of a tender irreducible groin mass with or without systemic signs of infection [12].
The choice of surgical approach for De Garengeot hernia remains controversial [13]. Classically, open inguinal or femoral operation was undertaken [9]. While effective, it has greater wound infection risks, particularly in the setting of acute appendicitis. Recently, minimal access techniques have been employed, with laparoscopy having several advantages [14]. A laparoscopic approach allows for complete inspection of the abdominal cavity, definitive diagnosis, and reduction of hernial contents and appendectomy can be safely performed [14]. Laparoscopy in our case provided a good view of the operating field, reduced surgical trauma, and expedited recovery.
The second crucial decision is whether to repair the hernia simultaneously as well. The acute inflammation in the context of possible use of prosthetic mesh complicates the risk of contamination and infection. Given that the burden of surgical site infection increases significantly after appendectomy, delay definitive hernia repair is advisable [15]. This approach minimizes the risk of prosthetic mesh infection and other postoperative complications. In our patient, this two-stage procedure was done, balancing the advantage of definitive hernia repair with the risk of postoperative complications.
In summary, clinicians should maintain a high index of suspicion for De Garengeot hernia, even in unusual patient presentations. Preoperative diagnosis is best achieved with CT scans. Laparoscopic management remains a safe and effective approach, and performing hernia repair in a staged manner helps reduce infection risk. Reporting such rare and atypical cases is important to enhance awareness, support early recognition, and guide appropriate surgical management.
Conclusion
De Garengeot hernia with acute appendicitis is a rare surgical pathology, particularly in young males. This case highlights the diagnostic challenges and the importance of tailored surgical planning. Preoperative CT imaging facilitates accurate diagnosis, while a staged laparoscopic approach—addressing appendicitis first, followed by hernia repair—offers a safe, infection-minimizing, and effective treatment strategy.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
None declared.
Informed consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Ethical statement
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal. The patient's privacy and confidentiality have been maintained throughout the preparation of this manuscript.



