-
PDF
- Split View
-
Views
-
Cite
Cite
Ying Marlene Zhang, Ida Lykke Kolmos, Beatrice Dyring-Andersen, A rare case of schwannoma on the foot: diagnostic challenges and clinical management, Journal of Surgical Case Reports, Volume 2025, Issue 9, September 2025, rjaf701, https://doi.org/10.1093/jscr/rjaf701
Close - Share Icon Share
Abstract
Schwannomas are benign peripheral nerve sheath tumors commonly found on the head, neck, and extremities, but they rarely occur on the feet and toes. Here, we present a case report of a 70-year-old woman with an ulcerated tender mass with an uncommon location on the lateral aspect of the left fifth toe. The tumor was initially misdiagnosed as hyperkeratosis, delaying correct treatment. Histological reassessment confirmed the diagnosis, schwannoma, highlighting the clinical challenges with diagnosing schwannomas due to their nonspecific appearance, and in this case, unusual presentation on the toe.
Introduction
Schwannomas, also known as neurilemmoma, are rare, benign encapsulated peripheral nerve sheath tumours (PNST) of Schwann cell origin. The tumours primarily present on the head- and neck regions, arms, and legs [1, 2]. They are, however, rarely found on the feet. Even though a painful palpable mass is the most prevalent symptom, the tumors can sometimes be asymptomatic [1, 3, 4]. The schwannomas are often clinically mistaken for lipomas, epidermal cysts or vascular malformation due to their nonspecific clinical appearance [5]. Herein, we report one of the rare cases of schwannoma presenting on the foot.
Case report
A 70-year-old female presented at the hospital with a superficially ulcerated palpable mass of ~6 mm on the lateral aspect of the fifth left toe. The patient had noticed a slowly growing, indolent tumour 8 months prior, and received a referral to a dermatologist who carried out a shave biopsy for diagnostic purpose. The first histological report described hyperkeratosis. The lesion was therefore treated with sharp debridement and more accommodative shoe wear and padding to relieve the mechanical stress in the area.
The lesion persisted and continued growing slowly, and the patient was therefore referred to a hospital department 3 months later. On examination, the patient presented a 3 mm ulceration with a slightly larger mobile, subcutaneous mass, tender to palpation (Fig. 1A). Examination with dermoscopy showed no signs of pigmentation or vascular structures (Fig. 1B). No other lesions were present on the skin upon clinical examination. The patient had sensations of tingling along the lateral side of the toe when the lesion was knocked, but was otherwise asymptomatic and had, apart from systemic sclerosis, no relevant past medical or family history.
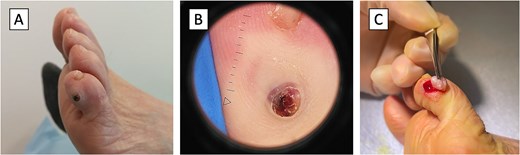
Schwannoma, the clinical presentation. (A) The patient presented with an ulcerated palpable round mass measuring 6 mm located on the lateral aspect of the fifth left toe. (B) Dermoscopy of the schwannoma showed a 3 mm ulceration with no pigmentation or vascular structures. (C) Excision of the tumor revealed an encapsulated, well-circumscribed schwannoma.
Histological assessment of the biopsy, and later the excision (Fig. 1C), revealed an encapsulated, well-circumscribed mass of spindle-shaped cells arranged in a cellular Antoni A pattern (Fig. 2A and B). Immunohistochemically, the tumor was positive for S100 and SOX10 (Fig. 2C and E, respectively), and negative for EMA, CD34, CKAE, Melan-A, and NF (Fig. 2D, F–I) [6].
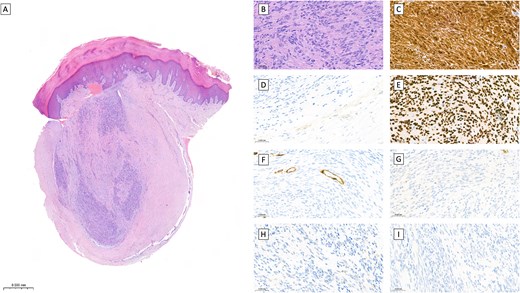
Schwannoma, the histological findings. Hematoxylin and eosin staining (A, B) and immunohistochemical staining (C–I) of the excised schwannoma. Overview of the excised schwannoma, bar = 0.5 mm (A). Histological image from the schwannoma with Antoni A pattern. The spindle-shaped cells show discreetly palisading arrangement around fibrillary processes (Verocay bodies) (B). The perineural capsule with positive immunoreactivity in EMA (D). The spindle cells are positive for S100 (C) and SOX10 (E) and negative for CD34 (F), CKAE (G), Melan-A (H) and NF (I). Magnification: (B–I) ×400.
Discussion
This case highlights the diagnostic challenges associated with schwannomas presenting in an atypical location. Our patient’s initial misdiagnosis as hyperkeratosis and subsequent treatment with debridement and the 3-month delay in definitive diagnosis underscores the importance of maintaining an awareness of soft tissue tumors as a potential cause of persistent lesions on the foot. While previous reports have successfully employed MRI and ultrasound for characterizing toe schwannomas, these imaging modalities were not utilized in our case. Advanced imaging could have potentially facilitated earlier diagnosis and guided appropriate tissue sampling through excisional rather than shave biopsy.
Differential diagnosis of soft tissue masses on the foot encompasses neurofibromas, lipomas, vascular malformations and, other PNST such as the malignant histological subtype - spindle cell sarcomas [7, 8]. Literature review revealed a few cases of digital schwannomas reporting similar symptomatic findings [8–10]. Previous studies have reported that schwannomas tend to be smaller in size and have fewer postoperative neurologic deficits than schwannomas at other anatomic sites [8]. This favourable profile likely reflects earlier clinical detection due to the mechanical stress and limited soft tissue coverage in this location. Schwannomas are also associated with the autosomal dominant disease neurofibromatosis type 2 (NF2). A population-based study of NF2-associated schwannomas reported that ~3% (12 of 455) of the patients with schwannoma presented with multiple schwannomas in association with NF2 [11]. Genetic factors should therefore always be considered when patients present with multiple nodules.
This case reinforces the clinical principle that persistent or growing masses warrant histopathologic evaluation beyond superficial sampling. While schwannomas are benign tumors with excellent prognosis following complete excision, accurate diagnosis remains essential to exclude malignant mimics and guide appropriate management. Our experience adds to the limited literature on digital schwannomas and emphasizes the importance of maintaining diagnostic vigilance when evaluating unusual soft tissue lesions of the foot.
Conflict of interest statement
None declared.
Funding
None declared.
References
Elder DE, Massi D, Scolyer RA, et al.



