-
PDF
- Split View
-
Views
-
Cite
Cite
Julia Todderud, Arvin Gee, Duy Nguyen, Case study: robotic foreign body removal of bullet in the aortopulmonary window, Journal of Surgical Case Reports, Volume 2025, Issue 9, September 2025, rjaf652, https://doi.org/10.1093/jscr/rjaf652
Close - Share Icon Share
Abstract
This case study reports on a 17-year-old male that underwent robotic assisted foreign body removal after sustaining a gunshot wound to the left upper arm that resulted in the bullet traversing through the chest wall to stop directly in the mediastinum at the aortopulmonary window. The proximity of the foreign body to the great vessels introduced challenges for preoperative imaging and surgical planning, thus becoming the focus of this unique case. Ultimately, the robotic-assisted removal of the bullet was successful without damage to the surrounding structures. To date, no known study has reported on robotic foreign body removal at this anatomic location.
Introduction
While gunshot wounds affecting the mediastinum are relatively rare, they carry a high mortality rate and present significant clinical challenges due to the critical structures in this region [1]. Existing literature discussing similar cases is limited, with relatively few studies reporting on transmediastinal injury and management. Degiannis et al. reported on patients with a range of transmediastinal injuries and injury mechanisms: urgent thoracotomy was performed on 51 patients, 27 with mediastinal injury [2]. In this cohort, 23/27 patients died perioperatively (85%) [2]. In another retrospective series, the overall mortality for transmediastinal gunshots was 79%, but only 24.3% for those who reached the hospital with vital signs [3]. Pediatric outcome studies are limited, with one study reporting 50% of the children requiring surgery following thoracic gunshot wounds and all deaths due to mediastinal injury [4].
The workup of mediastinal penetrating trauma favors CT imaging for guiding management in stable patients, with advantages for indicating trajectory and assessing extent of injury [5–9]. Management recommendations are widely varied between injury patterns and affected structures, but generally focuses on efficiency and caution [1].
The aortopulmonary window represents a high-risk narrow space between the inferior aspect of the aortic arch and the superior aspect of the pulmonary artery. With the entire body’s blood volume passing through these adjacent structures, injury to them would have high risk for catastrophic hemorrhage. Even when hemodynamically stable, leaving the foreign body in place runs the risk of erosion, migration, or embolization [1, 10]. Cardiac motion and vessel movement significantly increase this risk, as ongoing motion and friction from the bullet can wear against the vessel walls. Intrathoracic bullet migration has been the subject of previous case studies with transit of the bullet through the vascular network [11–14].
With this study we focus on this incredibly rare injury pattern: a gunshot wound resulting in a bullet lodged in the aortopulmonary window of a pediatric patient who underwent successful robotic surgery to extract the retained bullet.
Case report
Patient presentation
The patient was a 17-year-old male that presented in the emergency department following a gunshot wound to the left upper extremity and chest while being a passenger in a vehicle. At his initial examination in the trauma bay, he was communicative and endorsed pain at the injury site on the left arm and pectoralis but did not have difficulty breathing or additional chest pain. He reported no medical or surgical history. The patient was 6′2″ and 220 pounds, with stable vitals within normal ranges, apart from elevated blood pressure and pulse. On physical exam, he had a regular rate and rhythm with normal heart sounds and clear lungs. Peripheral pulses were 2+ and his skin was warm and dry. The gunshot wound was localized to the lateral aspect of his left upper arm: a 1 × 2 cm ovoid laceration with minimal hematoma and slight venous ooze.
Trauma workup imaging began with a chest X-ray (CXR), triggering a chest CT given the bullet’s location in the mediastinum. With the bullet near the great vessels, a transthoracic echocardiography (TTE) and a CT using a cardiac gated/dissection protocol were obtained. The visualization of vasculature and normal anatomy was limited by metallic artifact from the foreign body (Fig. 1). The chest CT demonstrated the largest bullet fragment located in the region of the aortopulmonary window, with no measurable distance between the bullet fragment and inferomedial margin of the aortic arch (Fig. 2). Less than 2 mm of separation was visualized between the bullet and the superior aspect of the left main pulmonary artery (Fig. 2). There was no contrast extravasation from the vasculature to suggest active bleeding, and there was no obvious mediastinal fluid collection / hematoma. TTE also visualized the aortic arch and showed no clear injury with laminar flow across the aorta. His initial CXR demonstrated a normal cardio-mediastinal silhouette (Fig. 1a). A small pneumothorax was seen with 2 mm pleural separation but repeat CXR did not indicate expansion, so chest tube placement was deferred (Fig. 1a and b). Upper extremity imaging suggested soft tissue laceration and bullet trajectory without arterial damage.
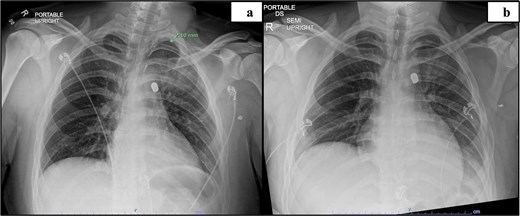
Preoperative imaging indicating the location of the projectile and image obstruction by metal artifact: Initial CXR (a), day 2 CXR (b).
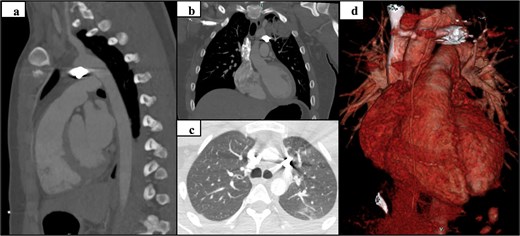
Preoperative CT and 3D reconstruction: sagittal (a), coronal (b), axial (c), and 3D reconstruction (d).
Preoperative counseling with the patient and his family discussed the options of leaving the bullet in, with a focus on unknown risk for bullet migration especially in a person so young with his entire life ahead of him. The constant motion of the pulmonary artery and aorta against the bullet raised significant concern of erosion into the vessels over time. Surgical options discussed included video assisted thoracoscopic surgery (VATS), thoracotomy, and sternotomy. While considering course of management, the patient underwent daily radiographs to assess for bullet migration, which did not occur. He remained stable for the preoperative course before proceeding with the surgical plan for flexible bronchoscopy, robotic left VATS, and extraction of the foreign body, with possible need for thoracotomy, aorta repair, and sternotomy.
Surgical procedure
The patient underwent surgery day 6 following admission. The surgical team included the primary thoracic surgeon, two cardiothoracic surgeons, and a first assist PA. He was intubated with a flexible double lumen endotracheal tube. Two large bore IVs, arterial line, right internal jugular venous line, and a Foley catheter were placed. The patient was positioned supine with a left chest bump. Given the location of the bullet and risk of injury to the great vessels, a sternal saw, cardiopulmonary bypass pump, cell salvage system, and two units of packed red blood cells were all set and ready for use in an emergency.
The decision was made to begin with VATS with potential to continue with VATS, or proceed with robotic VATS, thoracotomy, or sternotomy depending on the operative findings. A 2 cm incision was made in the anterolateral fifth intercostal space and a GelPoint mini wound protector was placed. An 8 mm 30-degree robotic camera was used and placed in the pleural space. There was no hemothorax. The left upper lobe trisegment was moderately ecchymotic with an intraparenchymal hematoma and was adhered to the superior mediastinum. The surgical team confirmed the backup plan for hemorrhage control.
Three 8 mm robotic ports were placed: #1 in the 5th intercostal space anterior to the GelPoint, #2 in the 5th intercostal space/midaxillary line, and #3 in the third intercostal space/midaxillary line. The GelPoint cap was placed with a 10 mm port and insufflation was initiated at 8 mmHg. At this time, 100 ml of bright clotted blood was visualized in the inferoposterior mediastinum. It was unclear if this blood originated from the lung or mediastinum but was not associated with trochar placement and did not reaccumulate. The GelPoint cap was removed and insufflation was discontinued for placement of a sponge stick for manipulation of the lung and for compression of any active bleeding. The lung was carefully peeled off the superior mediastinum without hemorrhage and was inspected. Port #3 was removed and the incision was widened to allow for finger placement and manual palpation of the lung, which indicated no bullet trapped in the lung tissue. Intraoperative radiography confirmed that the bullet was still in the mediastinum (Fig. 3b). The surgical team then deemed it to be safe to proceed with robotic VATS.
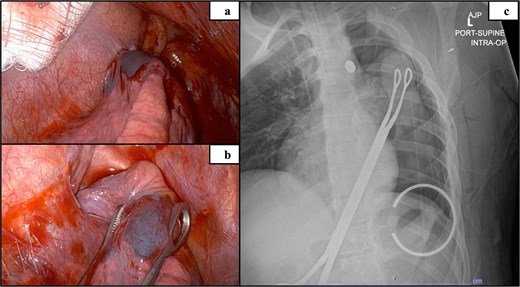
Intraoperative mediastinum adhesion visualized via robot (a), isolated upper lobe suspicious of containing bullet remnant (b) and intraoperative radiograph confirming bullet localized in the mediastinum (c).
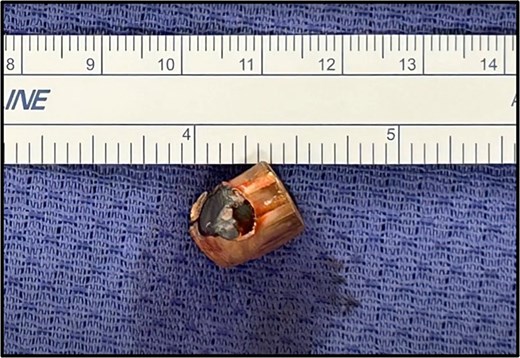
All ports were placed and insufflation was restarted. The robot was docked and instruments were placed. The left arm (Port #1) used a tip-up grasper and the right arm (Port #3) used a long bipolar dissector. The 5 mm mediastinal defect was inspected; the phrenic nerve was directly posterior to the injury. The mediastinal pleura was opened longitudinally above and below the defect (Fig. 4a). A small amount of turbid fluid was evacuated, and the metal foreign body was identified (Fig. 4a and b). With gentle manipulation, the foreign body was rotated, indicating it was not lodged in a structure (Fig. 4c). There was no bleeding to indicate vascular injury. The foreign body (Fig. 4d and e) was grasped and removed in its entirety without damage to surrounding structures. The mediastinal defect was hemostatic and no further dissection was performed. A posterior intercostal nerve block was performed on the intercostal spaces 4–11, and cryoablation of the intercostal nerves level 5–11. The instruments, camera, and sponge were removed, and the robot was undocked. A 24Fr chest tube was placed, the lung was inflated, the chest was closed, and the patient was extubated. The estimated blood loss was 10 ml. The operative time was 1 hour 38 minutes. The foreign body (Fig. 5) was sent to the appropriate authorities.
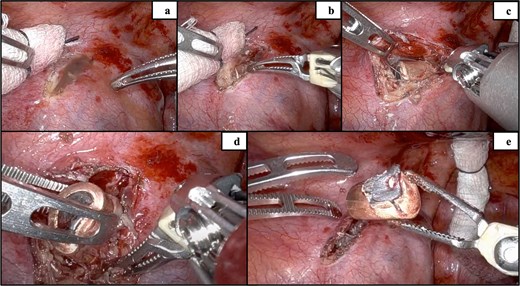
Incision of the mediastinal pleura (a), initial visualization of the bullet (b), dissection of the pleura (c), removal of the bullet (d), and confirmation of no bleeding with the bullet removed (e).
Post-operative course
The patient was discharged on post-operative Day 1 following chest tube removal with minimal output and no air leak; his discharge was Day 7 following the initial injury and admission. He was stable without acute concerns and was discharged home. At his 2 week follow-up, he was doing well without pain or shortness of breath (Fig. 6).

Discussion
This patient was incredibly fortunate regarding the bullet position, as any further propulsion would have likely penetrated the vasculature with subsequent catastrophic hemorrhage. The surgical team accounted for potential vasculature involvement, and the operating room was prepped in consideration of potential emergent conversion to open sternotomy. This study shares the limitations common to case study design, as it reports on a single instance of a rare trauma condition and subsequent management. While this study reports on a pediatric patient, the patient’s size would be consistent with adult management. This case describes a novel instance of robotic assisted foreign body removal from the aortopulmonary window, without vascular compromise following a gunshot wound to the left upper extremity and chest.
Conflict of interest statement
None declared.
Funding
None declared.



