-
PDF
- Split View
-
Views
-
Cite
Cite
Abdulaziz S AlQahtani, Saleh Husam Aldeligan, Abdulaziz Abdulmuhsin Alqusiyer, Abdullah Aljunaydil, Budur T Althobaiti, Areej Bokhari, Chest wall and axillary lipomatosis in association with cystic hygroma, thyroid nodules, and vascular complications—a comprehensive case study, Journal of Surgical Case Reports, Volume 2025, Issue 9, September 2025, rjaf378, https://doi.org/10.1093/jscr/rjaf378
Close - Share Icon Share
Abstract
Lipomas, benign proliferations of mature adipose tissue, are the most common subcutaneous mesenchymal tumors and typically remain asymptomatic unless they enlarge significantly or involve critical structures. Lipomatosis, the diffuse formation of multiple lipomas, is a rare condition that can affect atypical anatomical sites, posing diagnostic and therapeutic challenges. We present a rare case of a 22-year-old female with diffuse lipomatosis involving the thyroid, axilla, anterior chest, and left breast, presenting with progressive swelling, compressive symptoms, and functional limitations. Imaging and histopathology confirmed benign adipose proliferation without malignancy. Surgical management included total thyroidectomy, level V neck dissection, and excision of 13.57 kg of lipomatous tissue. Postoperatively, the patient developed a left upper limb deep vein thrombosis (DVT), successfully managed with anticoagulation. Follow-up showed no recurrence or residual lipomatosis. This case highlights the unusual presentation of extensive lipomatosis involving the thyroid and emphasizes the need for thorough diagnostic workup and careful surgical planning to optimize patient outcomes.
Introduction
Lipoma, a proliferative mass of mature adipose tissue, is the most common benign subcutaneous tumor and the most prevalent mesenchymal tumor in the human body. Histopathologically, it is classified into mature (lipoma) and immature (lipoblastoma), the latter often considered malignant. Vascular involvement may result in thrombosis, forming an angiolipoma [1]. The etiology of lipoma remains unclear but is likely multifactorial. Trauma to subcutaneous tissues may induce fat necrosis and local inflammation, triggering adipose proliferation [2], while genetic predisposition has also been implicated [3]. The malignant potential of lipomas remains debated. Some studies suggest a risk of transformation involving bone invasion [4], though evidence is conflicting. Malignancy risk depends on histopathological features, genetic alterations, anatomical site, and degree of invasion. Typically, lipomas are indolent and asymptomatic until they reach a substantial size [5]. They rarely cause complications but may lead to cosmetic concerns, particularly in the neck region of female patients. Deep-seated lipomas within muscle layers or fascial compartments are uncommon but may cause pain, pressure symptoms, or neurovascular compression [6]. Beyond subcutaneous locations, lipomas can involve the thyroid, retroperitoneum, deep neck structures, and brachial plexus [7]. Lipomatosis, the diffuse formation of multiple lipomas, can significantly impair quality of life [8], resulting in movement restrictions, neurovascular symptoms, and esthetic issues. It may also appear as part of metabolic syndromes classified under lipodystrophy [9]. An extreme case documented a 23.35 kg lipoma over 30–35 years, displacing the brachial plexus and infiltrating neurovascular structures, where surgical resection was incomplete due to nerve involvement, illustrating the potential for massive growth. Although differential diagnoses are few, excluding malignancies such as liposarcoma, lymphoma, angiosarcoma, and metastases is crucial. Benign mimickers include epidermal cysts, hibernomas, fat necrosis, and abscesses [10]. Diagnosis usually relies on clinical evaluation, supplemented by imaging for disease extension; biopsy is reserved for uncertain cases. Asymptomatic lipomas can be observed, but surgical excision with clear margins remains the definitive treatment to prevent recurrence. This case report presents a patient with extensive lipomatosis affecting the axillary, breast, thyroid, and neck regions, highlighting its surgical management.
Case presentation
A 22-year-old female presented with progressive swelling in the left anterior chest wall above the left breast, associated with needle-like chest pain, left upper limb tingling, and weakness. The patient had a history of childhood cystic hygroma in the left axilla, previously excised. She denied constitutional symptoms but reported compressive symptoms such as shortness of breath, dysphagia, and hoarseness. A family history of breast cancer with thyroid metastasis was noted in her mother. On examination, the patient exhibited multiple bilateral solitary thyroid nodules and a bulky swelling in the left anterior chest and axilla. Computed tomography (CT) imaging (Fig. 1) revealed hypodense bilateral thyroid nodules, with magnetic resonance imaging (MRI) (Fig. 2) showing an enhancing left axillary lesion (2 cm, previously 1 cm) and an anterior chest wall lesion (1 cm). The mass, measuring 23 × 8 cm, extended to the lower left neck, left chest wall, and left axilla, encasing the neurovascular bundle without muscle or osseous invasion (Fig. 3). Fine-needle aspiration (FNA) cytology (Fig. 4) of the right thyroid nodule indicated atypia of undetermined significance (Bethesda III), while left-sided nodules and biopsies from the axilla, breast, and neck confirmed benign mature adipose tissue. The patient underwent total thyroidectomy, level V left neck exploration, and excision of lipomatous masses from the axilla, anterior chest, and breast, involving multiple surgical teams. Intraoperatively, vocal cords were preserved, and clear planes for lipoma excision were identified. The total excised lipomatous tissue weighed 13.57 kg (Fig. 5). Pathological examination confirmed mature adipose proliferation with no malignancy. Fluorescence in situ hybridization (FISH) ruled out MDM2 amplification, and genetic testing returned negative. Postoperatively, the patient developed deep vein thrombosis (DVT) in the left upper limb, diagnosed via Doppler study, and was treated with low-molecular-weight heparin (LMWH) followed by rivaroxaban. Follow-up MRI at 2 days and 3 months confirmed no residual or recurrent tissue growth. The patient started levothyroxine for thyroid function management and monitored for optimal dosing.

Interval increase in size of the large left upper lateral cervical, sub-pectoral, and axillary region fatty lesion protruding beyond the pectoralis major muscle into the upper breast region, keeping with lipomatosis.
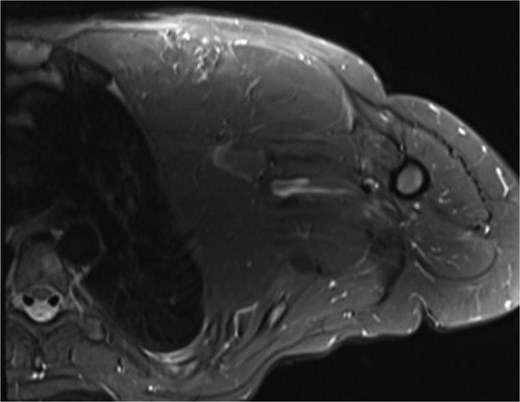
Left chest wall lipomatosis with extension to the left neck and left axilla with thin septations, and there is a small enhancing focus (within the fatty lesion) which could be a small enhancing nodule or lymph node. The overall measurement has relatively increased (consider patient maturation).
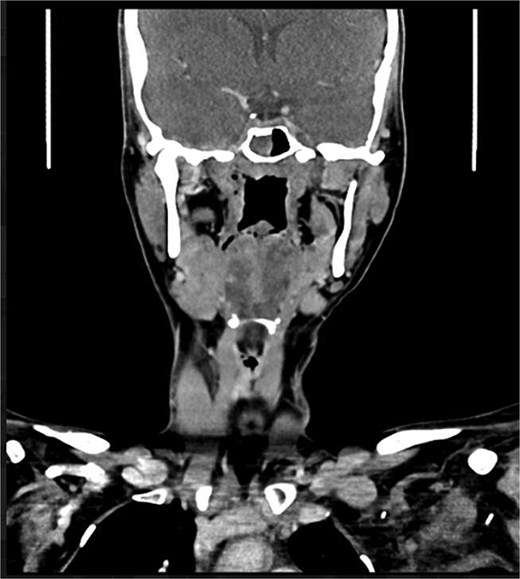
Partially scanned left thoracic lipomatosis extending to the lower neck with mild mass effect over the left internal jugular vein. A multilocular goiter with a complex thyroid nodule is noted in the lower neck.
![(A) Benign mature adipose tissue [Hematoxylin and eosin (H&E) 40×]. (B). Focal benign lipomatous changes in the thyroid gland (H&E 40×). (C). Focal benign lipomatous changes in the lymph node (H&E 40×).](https://oupdevcdn.silverchair-staging.com/oup/backfile/Content_public/Journal/jscr/2025/9/10.1093_jscr_rjaf378/1/m_rjaf378f4.jpeg?Expires=1774108623&Signature=ejkk60T6m749wjAZlIIXx4C4gXadNGhRj2P6uYl6og5Gna4G~r3SRAikzGMrn-yCgBhQxMS5IPrFGYgM~OQH3YgronUgnpLNO1R22Qqgwbl7hdiYfZSCV4mHSFc3FVODKiETPHQ3rvPDYhCIp9LTMT53UOpVT-rv7I5iAcOHfyq0deRh9tgOFevkY8ETBpRS33R8SpTmffZB6Dh0ALBjqgHou-xQpmO4pgUEVatf3jp0b8yzEzb331ZeNkuasDSx2Givd1Uy-8ILct7Jk~IMEUqQS3sU7-tye-TaomXIueMYXjbn4nJXrvdE-yOa4LE63VZErZy9tTB4TRU3w54R5A__&Key-Pair-Id=APKAIYYTVHKX7JZB5EAA)
(A) Benign mature adipose tissue [Hematoxylin and eosin (H&E) 40×]. (B). Focal benign lipomatous changes in the thyroid gland (H&E 40×). (C). Focal benign lipomatous changes in the lymph node (H&E 40×).
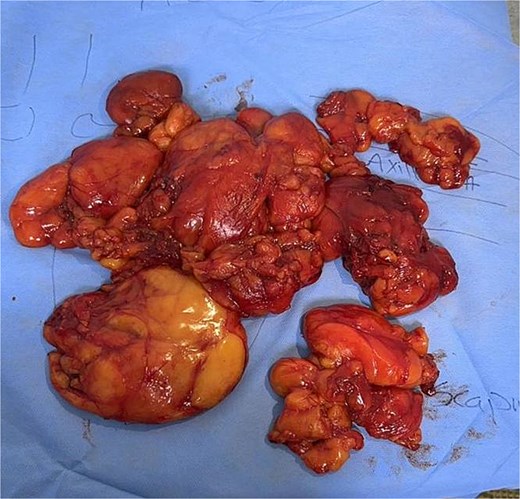
Multiple masses with fatty appearance (from neck, left axilla, and chest wall) ranging in size from 9.0 to 18.0 cm.
Discussion
The case delves into the complexities of adipose tissue and lipomatosis, a condition characterized by the formation of multiple lipomas in abnormal locations. Adipose tissue, primarily composed of adipocytes, is typically found in the breast, abdominal cavity, and internal organs. However, lipomatosis presents a rare scenario with a 10% incidence of lipomas formed in abnormal locations [11]. Despite extensive research, the underlying causes of lipomatosis remain elusive. Theories propose a potential association between physical trauma and the formation of lipomas [12]. Notably, lipomas predominantly affect the extremities and trunk [8], although adipose tissue in the thyroid is an uncommon occurrence [13]. Dhayagude’s research in 1942 marked the first reported instance of abnormal diffused adipose tissue in the thyroid gland [14]. When adipose tissue is identified in the thyroid, careful consideration must be given to ruling out various conditions, including papillary carcinoma [14], adenolipoma, and the exceptionally rare diffuse infiltration of fat [15]. The rarity of axillary lipomas is underscored by a case presenting 31 cases of masses in the axillary region, with only one being a lipoma [16]. Diagnosing such conditions that manifest in diverse locations necessitates advanced imaging modalities. CT scans and MRIs have emerged as the preferred diagnostic tools due to their ability to provide comprehensive information [17]. While ultrasound can be utilized, its limitations in revealing detailed structures make it a less favorable option. Treatment strategies for lipomatosis involve surgical excision or liposuction as an alternative approach. Surgical excision, the preferred method, aims to minimize complications related to potential injury to nerves and vessels [2]. Alternatively, liposuction serves as a viable option for patients concerned about scarring resulting from traditional incision-based surgery. In expanding the discourse, this case introduces a rare form of extensive lipomatosis with multi-locational involvement, including the thyroid, axilla, chest, and breast. It’s also worth noting the huge size of the total lipomatous tissue excised, weighing 13.57 kg, which is, to our knowledge, the largest amount of lipomatous tissue ever excised. The patient underwent total thyroidectomy, level 5 neck dissection, and axillary exploration to excise all affected tissues. Although the postoperative period was generally uneventful, the patient experienced left upper limb DVT, managed with rivaroxaban. Subsequent follow-up in our clinic, coupled with imaging studies, revealed no signs of pathological findings, demonstrating the efficacy of the intervention. This case contributes valuable insights into the understanding and management of lipomatosis, shedding light on its diverse manifestations and emphasizing the significance of accurate diagnosis and appropriate treatment modalities. The rarity of the reported case underscores the need for continued research to unravel the complexities of lipomatosis and its varied presentations across different anatomical locations.
Acknowledgement
The authors would like to acknowledge Professor Hamad AlJaedi, Department of Pathology, College of Medicine and King Saud University Medical City, King Saud University, Riyadh, Saudi Arabia, for his valuable contribution to this case report. Professor AlJaedi conducted the histopathological evaluation of the excised specimen, provided detailed pathology descriptions, and prepared the pathological images that were included in the manuscript. His expert input greatly enhanced the diagnostic confirmation and scientific quality of this work.
Conflict of interest statement
None declared.
Funding
None declared.



