-
PDF
- Split View
-
Views
-
Cite
Cite
Andrew Kerner, Galen Garriga, Dasiel B De Luna, Samuel De Jesus, Antonio Caycedo-Marulanda, Surgical management of incarcerated cecostomy intussusception following refractory acute colonic pseudo-obstruction, Journal of Surgical Case Reports, Volume 2025, Issue 8, August 2025, rjaf643, https://doi.org/10.1093/jscr/rjaf643
Close - Share Icon Share
Abstract
Acute colonic pseudo-obstruction (ACPO), or Ogilvie’s syndrome, is a rare but serious condition of colonic dilation without mechanical obstruction. Management becomes increasingly complex in patients with significant baseline comorbidities. We describe a 69-year-old female with extensive comorbidities who presented with acute on chronic hypoxic respiratory failure due to influenza pneumonia. During a prolonged ICU course, she developed progressive abdominal distension and was diagnosed with ACPO refractory to conservative and pharmacologic management. The patient was taken to surgery where a cecostomy was matured. Subsequently, she developed an incarcerated cecostomy intussusception. Surgical exploration revealed chronic right colon dilation and cecal prolapse, prompting a right hemicolectomy with end-ileostomy. This case highlights the role of stepwise surgical intervention in refractory ACPO, particularly in medically complex patients. While cecostomy may serve as a temporizing measure, complications such as intussusception may necessitate definitive resection. A tailored surgical approach is essential for optimizing outcomes.
Introduction
Acute colonic pseudo-obstruction (ACPO), or Ogilvie’s syndrome, is a functional disorder characterized by marked colonic dilation in the absence of mechanical obstruction. First described by Sir William Ogilvie in 1948, ACPO primarily affects hospitalized or critically ill patients and is associated with predisposing factors such as severe systemic illness, metabolic disturbances, trauma, recent surgery, or neurologic disease [1]. The pathophysiology is thought to involve an imbalance in autonomic regulation of colonic motility, particularly a suppression of parasympathetic activity, resulting in colonic atony and progressive distension most commonly affecting the cecum and ascending colon [2]. Initial management focuses on supportive measures including bowel rest, correction of electrolytes, and reduction of narcotic or anticholinergic medications. In patients who fail to improve, pharmacologic therapy with intravenous neostigmine, an acetylcholinesterase inhibitor, has demonstrated clinical success rates of up to 80%–90% in selected populations [3]. Endoscopic decompression represents an alternative for those who do not respond or have contraindications to pharmacologic treatment. A small subset of patients remains refractory to both medical and endoscopic therapies, especially in the presence of progressive dilation, suspected ischemia, or clinical deterioration. In such cases, surgical intervention may become necessary. While colectomy is reserved for frank ischemia or perforation, minimally invasive decompression via surgical or percutaneous cecostomy has been employed as a temporizing or definitive strategy in high-risk patients [4]. However, as per the ASCRS Clinical Practice Guidelines for the management of ACPO, there is no standardized approach to for the surgical management in refractory cases [5].
Case report
A 69-year-old female with significant comorbidities including chronic obstructive pulmonary disease (COPD), congestive heart failure with pacemaker, chronic kidney disease, acute myeloid leukemia (status post bone marrow transplant), and squamous cell carcinoma of the head and neck (status post-radiation) presented on February 5, 2025, with acute on chronic hypoxic respiratory failure secondary to influenza pneumonia in the setting of a COPD exacerbation.
Despite aggressive respiratory support, her clinical course necessitated prolonged intubation and eventual tracheostomy placement. During her ICU stay, she developed progressive abdominal distension. Imaging revealed colonic ileus, with concern for distal obstruction. Gastroenterology administered neostigmine on two occasions without clinical improvement. Worsening abdominal distension and exam findings prompted further imaging, which demonstrated cecal pneumatosis with suspicion of ischemia (Fig. 1).

Development of cecal pneumatosis after administration of neostigmine.
Colorectal surgery was then consulted, and the patient underwent diagnostic laparoscopy on March 1, 2025. Intraoperative assessment showed a viable cecum and ascending colon without gross evidence of serosal tears or ischemia. Given the refractory nature of her pseudo-obstruction, a cecostomy was created in the right lower quadrant. Colonic resection was considered but given her comorbidities and nutritional status, a cecostomy was felt to be a safer therapeutic option. Her postoperative recovery was uncomplicated from a surgical standpoint, with resolution of abdominal distension and return of bowel function. She was discharged to long-term acute care (LTAC) on March 7, 2025, for ongoing ventilatory support.
On March 11, 2025, the patient was readmitted in septic shock due to pseudomonal pneumonia and an acute gastrointestinal bleed. She suffered a cardiac arrest on arrival and was successfully resuscitated. A pigtail chest tube was placed for an iatrogenic pneumothorax incurred during resuscitation. Imaging demonstrated bilateral pneumonia, pneumoperitoneum, possible portal venous thrombosis, and suspected enterocolitis. Although general surgery recommended operative intervention, the family declined at that time.
She was managed in the ICU with intravenous antibiotics and hemodynamic support. Colorectal surgery was reconsulted for persistent gastrointestinal bleeding. Bedside colonoscopy identified no intraluminal source but did reveal a mucosal bleed at the cecostomy site, managed with topical hemostatic agents. Her hemodynamics stabilized, though her respiratory failure persisted as the primary barrier to recovery.
Soon thereafter, a large prolapse of the cecostomy site was noted (Figs 2 and 3). Conservative measures including manual reduction and hyperosmotic agents were unsuccessful. On April 15, 2025, she was taken to the operating room. Diagnostic laparoscopy revealed a small fascial defect at the cecostomy site with cecal intussusception. The fascial defect was extended cephalad, and the prolapsed cecum was successfully everted and reduced (Fig. 4). Due to the chronically dilated right colon and the patient’s history of refractory ACPO, a right hemicolectomy with end-ileostomy was performed.

Anterior/posterior view of incarcerated cecostomy intussusception.

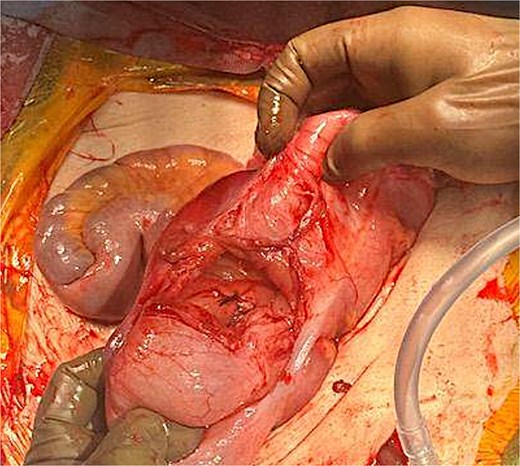
Successful eversion and reduction of cecostomy intussusception.
Her postoperative recovery was uncomplicated. The ileostomy functioned appropriately, she tolerated enteral nutrition, and no abdominal complications developed. She remained hospitalized for continued management of respiratory failure.
Discussion
This case highlights the complex decision-making required in the management of ACPO, particularly in patients with multiple severe comorbidities. While conservative, pharmacologic, and endoscopic measures are frequently effective, this patient’s refractory course necessitated escalation to surgical intervention.
Initial diagnostic laparoscopy confirmed a viable colon, and a cecostomy provided effective decompression. However, the patient subsequently developed cecostomy prolapse and intussusception, which is an uncommon but recognized complication in debilitated patients with chronically distended, atonic colons and poor tissue integrity. These findings ultimately warranted definitive resection via right hemicolectomy and end-ileostomy.
The decision to proceed with colectomy was informed by intraoperative evidence of chronic right-sided colonic dilation and the high likelihood of recurrence. This approach, while aggressive, was thought to be an appropriate escalation given the patient’s clinical trajectory and persistent critical illness.
Importantly, this case underscores the value of maintaining surgical flexibility and multidisciplinary collaboration in medically fragile patients. Despite significant physiological compromise, the patient experienced a favorable postoperative course, emphasizing that selected high-risk individuals may still benefit from timely and targeted surgical intervention.
This case illustrates the importance of a tailored, stepwise approach to ACPO management. It reinforces the utility of cecostomy as both a diagnostic and therapeutic tool and highlights the need for vigilance in recognizing and addressing rare but serious complications such as cecostomy-associated intussusception.
Conclusion
In medically complex patients with refractory ACPO, minimally invasive interventions can provide both diagnostic insight and therapeutic decompression. Cecostomy remains a valuable option for temporary relief in high-risk individuals; however, close surveillance is essential to detect complications such as prolapse or intussusception. In cases of chronic colonic dysmotility or anatomical compromise, definitive surgical resection may be warranted. This case highlights the importance of a tailored, stepwise surgical approach and underscores the role of interdisciplinary coordination in achieving favorable outcomes, even in physiologically fragile patients.
Conflict of interest statement
None declared.
Funding
None declared.



