-
PDF
- Split View
-
Views
-
Cite
Cite
Abdullah S Al-Darwish, Mohannad K Saffaf, Leen O Alothaim, Sami AlHawassi, A giant gastric trichobezoar requiring surgical intervention: a case report and literature review, Journal of Surgical Case Reports, Volume 2025, Issue 8, August 2025, rjaf641, https://doi.org/10.1093/jscr/rjaf641
Close - Share Icon Share
Abstract
We report the case of a 42-year-old female with a history of gastropexy for weight loss 5 years prior, who presented with chronic upper abdominal pain, nausea, and a palpable left upper quadrant mass. Imaging and endoscopic evaluation revealed a large trichobezoar occupying most of the gastric lumen. Due to its size and composition, endoscopic removal was unsuccessful, and surgical intervention was required. This case highlights the importance of considering bezoars in the differential diagnosis of vague gastrointestinal symptoms, particularly in patients with altered gastric anatomy or associated behavioral disorders.
Introduction
A bezoar is an intraluminal accumulation of indigestible or poorly digestible material within the gastrointestinal (GI) tract. While bezoars may occur anywhere along the GI tract, they are most commonly found in the stomach [1]. Gastric bezoars are rare, with an estimated incidence ranging from 0.4% to 1% in upper endoscopies performed for dyspepsia [1, 2]. In rare cases, bezoars can extend beyond the pylorus into the small intestine, a condition known as Rapunzel syndrome [2].
Bezoars are classified based on their composition. Phytobezoars, composed of indigestible plant fibers, are the most common type. In contrast, trichobezoars, which consist primarily of ingested hair, typically affect young female patients and are strongly associated with psychiatric conditions such as trichotillomania and trichophagia. The prevalence of trichophagia in patients with psychiatric disorders may reach up to 1% [1, 3].
Case presentation
A 42-year-old female, otherwise medically free except for mild iron deficiency anemia, with a surgical history of laparoscopic gastropexy 5 years ago for obesity [initial body mass index (BMI) 38 kg/m2, post-surgery BMI 27 kg/m2], presented with a 2-week history of vague, chronic upper abdominal pain, nausea, heartburn, and a palpable upper abdominal swelling. There were no constitutional symptoms such as fever or weight loss.
On examination, the abdomen was soft with a large, firm, non-tender mass in the left upper quadrant. Laboratory tests revealed mild anemia (Hb 10.8 g/dL), normal liver function tests, and normal renal function. Electrolytes and inflammatory markers were within normal limits.
A contrast-enhanced portal venous phase CT scan of the abdomen (Fig. 1a: axial section; Fig. 1b: coronal section) revealed significant gastric distension with a mixed-attenuation intragastric mass showing a whorled pattern and internal calcifications, consistent with a gastric bezoar [2, 4]. An upper gastrointestinal endoscopy confirmed a large trichobezoar occupying ˃90% of the gastric lumen (Fig. 2a and b). The mass was too large and dense for endoscopic removal.
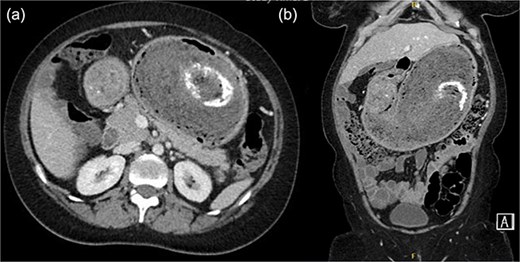
(a) Axial contrast-enhanced CT image of the abdomen showing a markedly distended stomach with a large intraluminal mass displaying a characteristic whorled appearance and internal foci of calcification (arrow), suggestive of a trichobezoar. (b) Coronal CT reconstruction demonstrating the full extent of the bezoar within the gastric lumen (arrow).
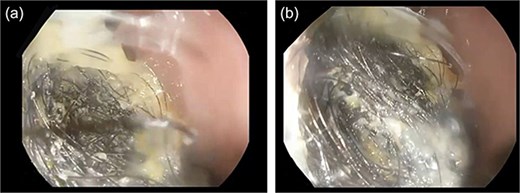
(a) Endoscopic view of the upper stomach showing a large, dense hairball (trichobezoar) occupying ˃90% of the gastric lumen. (b) Closer endoscopic image highlighting the compact hair fibers and matted texture preventing safe endoscopic extraction.
Due to the size of the bezoar, failed endoscopic extraction, and the need for psychiatric evaluation, the patient underwent Emergency laparotomy. Intraoperatively, the stomach was markedly distended. An 8 cm longitudinal gastrotomy was made along the greater curvature, and the bezoar was extracted en bloc (Fig. 3a–d). Gastric closure was achieved using a 75 mm gastrointestinal anastomosis stapler, reinforced with 2–0 Vicryl sutures in a Lambert fashion. A methylene blue test showed no leak.
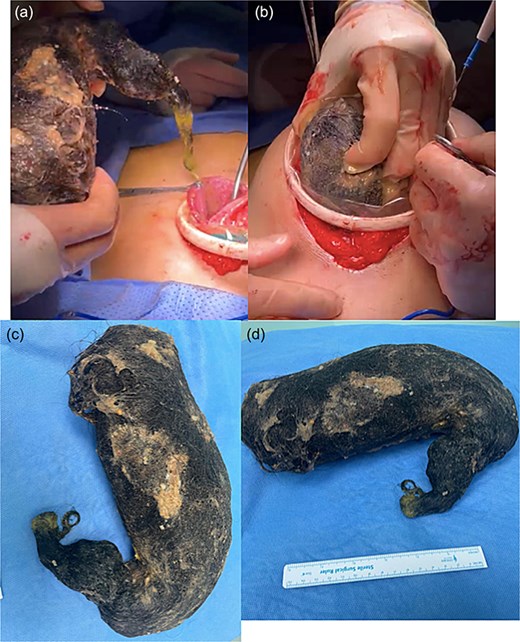
(a) Intraoperative view showing the distended stomach before gastrotomy. (b) Gastrotomy along the greater curvature with partial exposure of the trichobezoar. (c) Extraction of the bezoar as a single, intact mass. (d) Resected bezoar specimen laid out, demonstrating its size and typical hairball consistency.
Her postoperative course was uneventful. A Gastrografin study on postoperative day 2 showed no leakage or obstruction. The patient resumed oral intake and was discharged on postoperative day 3 with scheduled psychiatric follow-up.
Discussion
Gastric trichobezoars are uncommon but significant causes of upper GI symptoms [1, 3, 5]. Psychiatric disorders and previous gastric surgeries, such as gastropexy, are recognized risk factors due to their impact on gastric motility and emptying [1, 3]. Trichobezoars account for ⁓0.15% of all gastrointestinal foreign bodies. Most patients are young females, although adult cases have been reported [3, 6, 7].
CT scanning typically reveals the classic whorled intraluminal mass, while endoscopy confirms the diagnosis and can sometimes allow therapeutic extraction [2, 4, 8]. Enzymatic or chemical dissolution, including Coca-Cola lavage, is effective mainly for phytobezoars but not for trichobezoars due to their dense keratin matrix [4]. Endoscopic fragmentation may be feasible for small trichobezoars but is rarely effective for giant masses; surgical removal remains the treatment of choice [1, 3, 6, 9].
A review of similar cases is summarized in Table 1, highlighting patient demographics, bezoar size, treatment, and outcomes [10–12].
| Author (Year) . | Age/Sex . | Bezoar Type . | Size/Extent . | Treatment . | Psychiatric Follow-Up . | Outcome . | Reference . |
|---|---|---|---|---|---|---|---|
| Gorter et al. (2010) | 14/F | Trichobezoar (Rapunzel) | Large, extending into jejunum | Open gastrotomy | Yes | No recurrence | Pediatr Surg Int. 2010;26(5):457–63. [PMID: 20182836] |
| Ahmad et al. (2017) | 16/F | Trichobezoar (Rapunzel) | Giant, gastric + small bowel | Laparotomy | Yes | No recurrence | BMJ Case Rep. 2017;2017:bcr2017221083. [PMID: 29208632] |
| Oh et al. (2015) | 21/F | Trichobezoar | Large, stomach only | Laparoscopic gastrotomy | Yes | No recurrence | Ann Surg Treat Res. 2015 Jun;88(6):346–9. [PMID: 26161290] |
| Gonuguntla et al. (2004) | 23/F | Trichobezoar | Giant, stomach + duodenum | Open gastrotomy | Yes | No recurrence | J Am Coll Surg. 2004;198(5):694–6. [PMID: 15110815] |
| Ayoub et al. (2013) | 22/F | Trichobezoar | Large, stomach only | Endoscopic attempt failed, then laparotomy | Yes | No recurrence | Int J Surg Case Rep. 2013;4(5):442–4. [PMID: 23638302] |
| Deslypere et al. (2010) | 30/F | Trichobezoar | Stomach only | Laparoscopic gastrotomy | Yes | No recurrence | Case Rep Gastroenterol. 2010;4(1):29–35. [PMID: 21103287] |
| Yau et al. (2012) | 8/F | Trichobezoar | Rapunzel, stomach + ileum | Laparotomy | Yes | No recurrence | Hong Kong Med J. 2012;18(3):246–8. [PMID: 22665692] |
| Naik et al. (2017) | 12/F | Trichobezoar | Large, Rapunzel | Open gastrotomy | Yes | No recurrence | J Clin Diagn Res. 2017;11(6):PD03–PD04. [PMID: 28764227] |
| Tsoucalas et al. (2018) | 38/F | Trichobezoar | Large, stomach only | Open gastrotomy | Yes | No recurrence | Cureus. 2018;10(3):e2311. [PMID: 29732441] |
| Author (Year) . | Age/Sex . | Bezoar Type . | Size/Extent . | Treatment . | Psychiatric Follow-Up . | Outcome . | Reference . |
|---|---|---|---|---|---|---|---|
| Gorter et al. (2010) | 14/F | Trichobezoar (Rapunzel) | Large, extending into jejunum | Open gastrotomy | Yes | No recurrence | Pediatr Surg Int. 2010;26(5):457–63. [PMID: 20182836] |
| Ahmad et al. (2017) | 16/F | Trichobezoar (Rapunzel) | Giant, gastric + small bowel | Laparotomy | Yes | No recurrence | BMJ Case Rep. 2017;2017:bcr2017221083. [PMID: 29208632] |
| Oh et al. (2015) | 21/F | Trichobezoar | Large, stomach only | Laparoscopic gastrotomy | Yes | No recurrence | Ann Surg Treat Res. 2015 Jun;88(6):346–9. [PMID: 26161290] |
| Gonuguntla et al. (2004) | 23/F | Trichobezoar | Giant, stomach + duodenum | Open gastrotomy | Yes | No recurrence | J Am Coll Surg. 2004;198(5):694–6. [PMID: 15110815] |
| Ayoub et al. (2013) | 22/F | Trichobezoar | Large, stomach only | Endoscopic attempt failed, then laparotomy | Yes | No recurrence | Int J Surg Case Rep. 2013;4(5):442–4. [PMID: 23638302] |
| Deslypere et al. (2010) | 30/F | Trichobezoar | Stomach only | Laparoscopic gastrotomy | Yes | No recurrence | Case Rep Gastroenterol. 2010;4(1):29–35. [PMID: 21103287] |
| Yau et al. (2012) | 8/F | Trichobezoar | Rapunzel, stomach + ileum | Laparotomy | Yes | No recurrence | Hong Kong Med J. 2012;18(3):246–8. [PMID: 22665692] |
| Naik et al. (2017) | 12/F | Trichobezoar | Large, Rapunzel | Open gastrotomy | Yes | No recurrence | J Clin Diagn Res. 2017;11(6):PD03–PD04. [PMID: 28764227] |
| Tsoucalas et al. (2018) | 38/F | Trichobezoar | Large, stomach only | Open gastrotomy | Yes | No recurrence | Cureus. 2018;10(3):e2311. [PMID: 29732441] |
| Author (Year) . | Age/Sex . | Bezoar Type . | Size/Extent . | Treatment . | Psychiatric Follow-Up . | Outcome . | Reference . |
|---|---|---|---|---|---|---|---|
| Gorter et al. (2010) | 14/F | Trichobezoar (Rapunzel) | Large, extending into jejunum | Open gastrotomy | Yes | No recurrence | Pediatr Surg Int. 2010;26(5):457–63. [PMID: 20182836] |
| Ahmad et al. (2017) | 16/F | Trichobezoar (Rapunzel) | Giant, gastric + small bowel | Laparotomy | Yes | No recurrence | BMJ Case Rep. 2017;2017:bcr2017221083. [PMID: 29208632] |
| Oh et al. (2015) | 21/F | Trichobezoar | Large, stomach only | Laparoscopic gastrotomy | Yes | No recurrence | Ann Surg Treat Res. 2015 Jun;88(6):346–9. [PMID: 26161290] |
| Gonuguntla et al. (2004) | 23/F | Trichobezoar | Giant, stomach + duodenum | Open gastrotomy | Yes | No recurrence | J Am Coll Surg. 2004;198(5):694–6. [PMID: 15110815] |
| Ayoub et al. (2013) | 22/F | Trichobezoar | Large, stomach only | Endoscopic attempt failed, then laparotomy | Yes | No recurrence | Int J Surg Case Rep. 2013;4(5):442–4. [PMID: 23638302] |
| Deslypere et al. (2010) | 30/F | Trichobezoar | Stomach only | Laparoscopic gastrotomy | Yes | No recurrence | Case Rep Gastroenterol. 2010;4(1):29–35. [PMID: 21103287] |
| Yau et al. (2012) | 8/F | Trichobezoar | Rapunzel, stomach + ileum | Laparotomy | Yes | No recurrence | Hong Kong Med J. 2012;18(3):246–8. [PMID: 22665692] |
| Naik et al. (2017) | 12/F | Trichobezoar | Large, Rapunzel | Open gastrotomy | Yes | No recurrence | J Clin Diagn Res. 2017;11(6):PD03–PD04. [PMID: 28764227] |
| Tsoucalas et al. (2018) | 38/F | Trichobezoar | Large, stomach only | Open gastrotomy | Yes | No recurrence | Cureus. 2018;10(3):e2311. [PMID: 29732441] |
| Author (Year) . | Age/Sex . | Bezoar Type . | Size/Extent . | Treatment . | Psychiatric Follow-Up . | Outcome . | Reference . |
|---|---|---|---|---|---|---|---|
| Gorter et al. (2010) | 14/F | Trichobezoar (Rapunzel) | Large, extending into jejunum | Open gastrotomy | Yes | No recurrence | Pediatr Surg Int. 2010;26(5):457–63. [PMID: 20182836] |
| Ahmad et al. (2017) | 16/F | Trichobezoar (Rapunzel) | Giant, gastric + small bowel | Laparotomy | Yes | No recurrence | BMJ Case Rep. 2017;2017:bcr2017221083. [PMID: 29208632] |
| Oh et al. (2015) | 21/F | Trichobezoar | Large, stomach only | Laparoscopic gastrotomy | Yes | No recurrence | Ann Surg Treat Res. 2015 Jun;88(6):346–9. [PMID: 26161290] |
| Gonuguntla et al. (2004) | 23/F | Trichobezoar | Giant, stomach + duodenum | Open gastrotomy | Yes | No recurrence | J Am Coll Surg. 2004;198(5):694–6. [PMID: 15110815] |
| Ayoub et al. (2013) | 22/F | Trichobezoar | Large, stomach only | Endoscopic attempt failed, then laparotomy | Yes | No recurrence | Int J Surg Case Rep. 2013;4(5):442–4. [PMID: 23638302] |
| Deslypere et al. (2010) | 30/F | Trichobezoar | Stomach only | Laparoscopic gastrotomy | Yes | No recurrence | Case Rep Gastroenterol. 2010;4(1):29–35. [PMID: 21103287] |
| Yau et al. (2012) | 8/F | Trichobezoar | Rapunzel, stomach + ileum | Laparotomy | Yes | No recurrence | Hong Kong Med J. 2012;18(3):246–8. [PMID: 22665692] |
| Naik et al. (2017) | 12/F | Trichobezoar | Large, Rapunzel | Open gastrotomy | Yes | No recurrence | J Clin Diagn Res. 2017;11(6):PD03–PD04. [PMID: 28764227] |
| Tsoucalas et al. (2018) | 38/F | Trichobezoar | Large, stomach only | Open gastrotomy | Yes | No recurrence | Cureus. 2018;10(3):e2311. [PMID: 29732441] |
Long-term management should include psychiatric assessment and support to address underlying trichophagia and reduce the risk of recurrence [13].
Conclusion
This case illustrates the diagnostic and therapeutic challenges of giant gastric trichobezoars. A high index of suspicion is warranted in patients with vague GI symptoms and a history of gastric surgery or behavioral disorders. Early recognition and multidisciplinary treatment, including psychiatric care, are key to preventing complications and recurrence.
Conflict of interest statement
None declared.
Funding
None declared.



