-
PDF
- Split View
-
Views
-
Cite
Cite
Juraj Kolak, Ivan Romic, Hrvoje Silovski, Kristina Krzelj, Gallstone ileus associated with obstructive jaundice and intestinal ischemia: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 8, August 2025, rjaf544, https://doi.org/10.1093/jscr/rjaf544
Close - Share Icon Share
Abstract
Typical gallstone ileus includes small intestine obstruction caused by the gallstone passing from the gallbladder through the common bile duct (CBD). The case of gallstone ileus with simultaneous obstructive jaundice and intestinal ischemia is an extremely rare scenario. Computed tomography of the abdomen and pelvis is the method of choice for the diagnosis. While some cases may be treated conservatively, surgery is often required, with the approach tailored to the patient’s general condition and medical history. Hereby, we present a case of an 88-year-old lady with gallstone ileus, obstructive jaundice, and radiologic signs of intestinal ischemia. Urgent surgery revealed a 3 cm gallstone in the ischemic distal jejunum and another in the CBD. Cholecystectomy, duodenal wall repair, choledochotomy with stone extraction, and T-drainage were performed. The patient was discharged from the hospital on the 25th postoperative day, and 1 year after the surgery, is in good general condition.
Introduction
Gallstone ileus is an intestinal obstruction caused by a gallstone passing through a biliary-enteric fistula into the gastrointestinal tract. This entity occurs in 0.15%–1.5% of cholelithiasis cases and in ˂0.1% of all ileus cases, with a higher prevalence in women and the elderly [1]. The diagnosis may be challenging due to the variability of its presentation, especially in older patients in poor general condition and with the burden of past medical history. Common symptoms include nausea, poor appetite, vomiting, fever, abdominal pain, hematemesis, and weight loss [2]. However, the case of gallstone ileus associated with obstructive jaundice and intestinal ischemia is an extremely rare scenario and is reported in the literature only as occasional case reports. The treatment recommendations are poorly established and differ from case to case.
This article brings a case of successful surgical treatment of an 88-year-old lady with gallstone ileus associated with obstructive jaundice and intestinal ischemia.
Case report
An 88-year-old lady was admitted to our institution due to vomiting for 4 days and hematemesis on admission. The patient was icteric, hypotensive, with a distended abdominal wall and periumbilical pain on palpation. Her past medical history included permanent atrial fibrillation on warfarin, hypothyroidism, and chronic kidney disease. Laboratory testing revealed leukocytosis (leucocytes 13.3 × 109/L), normal hematocrit (0.36 L/L), elevated C-reactive protein level (CRP 89 mg/L), INR >6.0, glomerular filtration rate of 25 ml/min/1.73 m2, elevated bilirubin level (total bilirubin 57 μmol/L; reference range 3–20) as well as elevated hepatic aminotransferases [alanine aminotransferase 76 U/L (reference range 10–36), aspartate aminotransferase 113 U/L (reference range 8–30), gamma glutamyl transferase 54 U/L (reference range 9–35), alkaline phosphatase 87 U/L (reference range 64–153)]. Abdominal computed tomography (CT) scan showed intestinal obstruction in the jejunum caused by a gallstone, a gallstone in the dilated bile duct, stomach/jejunal dilatation and hepatic pneumobilia (Fig. 1). The patient received prothrombin complex concentrate, vitamin K, and other resuscitative measures before undergoing emergency surgery via median laparotomy. Intraoperatively, the small intestine was distended orally from the incarcerated 3 × 3 cm gallstone at 50 cm from the Treitz ligament and with subsequent tiger-stripe ischemic changes of the jejunum proximal to stone impaction (Fig. 2). Additionally, a cholecystoduodenal fistula and a 15-mm gallstone in the common bile duct (CBD) were found. The cholecystectomy and duodenal defect repair were performed. The gallstone was extracted from the CBD via choledochotomy and T-drainage. The ischemic part of the small intestine was resected, the gallstone was removed, and intestinal continuity was restored. Histopathology confirmed hemorrhagic necrosis of the resected intestine. After successful treatment, the patient was discharged home. One year after the surgery, the patient remained in good general health.
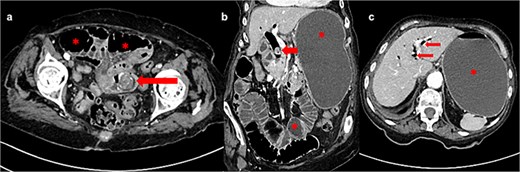
(a) Axial CT image shows gallstone in jejunum (arrow) and dilated bowel loops proximally (asterisk); (b) frontal CT image shows dilated stomach and bowel loops (asterisk) and gallstone in dilated common bile duct (arrow); (c) axial CT image shows pneumobilia (arrows) and fluid-filled and dilated stomach (asterisk).
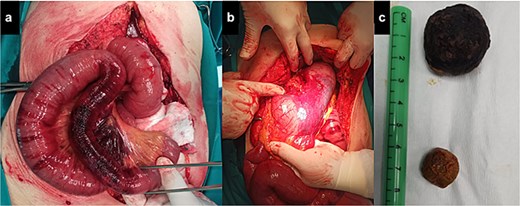
(a) Dilated bowel loops with ischemic part adjacent to the gallstone (pointed by grasper); (b) massively dilated stomach; (c) stones found in the jejunum (the larger one) and the common bile duct (the smaller one).
Discussion
The simultaneous occurrence of gallstone ileus, obstructive jaundice, and intestinal ischemia is very rare. Our patient had the obstruction of both, the intestinal and biliary tract with gallstones, one in the jejunum and another in the CBD, with cholecystoduodenal fistula as the cause of ileus. Because of nonspecific symptoms, diagnosis is not always straightforward. Jaundice in gallstone ileus is very rare and reported in only up to 15% of patients [2], as in most cases, bile may freely flow to the duodenum through the gallbladder and fistula even if there is a stone in the distal CBD.
Although ileus can be revealed on abdominal X-rays, in many cases, intestinal obstruction caused by a gallstone may not be confirmed using this diagnostic method. Therefore, the optimal method for establishing gallstone ileus is a contrast-enhanced abdominal-pelvic CT scan, which provides information on the cause and level of obstruction [1–3].
The treatment depends on the patient’s general condition and previous abdominal surgery [1]. Although spontaneous resolutions of gallstone ileus have been reported [4, 5], there are no specific recommendations for treatment. Surgery is indicated for cases of gallstone ileus and involves the extraction of the stone and closure of the fistula. Some sources recommend a one-stage surgical approach (enterotomy, fistula repair and cholecystectomy), whereas others advocate two-stage surgery (enterolithotomy and cholecystectomy in the first stage, followed by late repair of the biliodigestive fistula in the second stage) [1, 3]. There are less invasive alternatives, such as laparoscopic procedures, which require a specialist experienced in advanced laparoscopic surgery [6, 7], whereas endoscopic [8, 9] and extracorporeal shock wave lithotripsy [10] are associated with frequent failure and are not available in many hospitals. Considering the severe mortality of this condition, treatment options should be well-weighted, especially in vulnerable populations of older patients with a burdened medical history. We performed a single-stage surgery, including the extraction of the gallstone from the CBD, because there was a risk of cholangitis since the CBD stone was located proximal to the cystic duct. Additionally, there were signs of subacute cholecystitis and periduodenitis so we didn’t want to risk postoperative duodenal perforation. Although the outcome was successful, it cannot be concluded that our approach is applicable to all cases. It is important to report on rare cases of gallstone ileus associated with obstructive jaundice to accumulate knowledge in treating this unusual clinical scenario. Notwithstanding the variable clinical presentation, this diagnosis should be considered in patients with suspected acute abdomen. Although some cases may be managed conservatively, surgery is usually recommended and should be carefully considered, taking into account the general condition and medical history.
Conflict of interest statement
None declared.
Funding
None declared.



