-
PDF
- Split View
-
Views
-
Cite
Cite
Takahiko Sakuma, Koichi Ohmoto, Takeshi Ito, Nuck canal cyst: use of immunohistochemistry to reveal vestigial endometriosis hidden within mural granulation tissue, Journal of Surgical Case Reports, Volume 2025, Issue 8, August 2025, rjaf540, https://doi.org/10.1093/jscr/rjaf540
Close - Share Icon Share
Abstract
A case of a Nuck canal cyst (NCC) associated with vestigial endometriosis is presented. An ultrasound scan revealed a multicystic sac in the right groin of a 42-year-old woman who had experienced inguinal discomfort for over 5 years. A Marcy repair was performed on the inguinal lesion based on the clinical diagnosis of an inguinal hernia. The resected multicystic blind tube had a small protruding nodule on the cyst wall. Although this nodule was initially thought to be granulation tissue, detailed high-power histological examination revealed severely degenerated residual glands that could not be characterised further using haematoxylin and eosin staining. Immunohistochemical staining revealed that the glandular epithelial cells were oestrogen receptor positive, while the background stromal cells were CD10 positive. A diagnosis of NCC with endometriosis was made. A review of the relevant literature concerning the complication of the NCC and the usefulness of immunohistochemical staining is also included.
Introduction
The canal of Nuck is a rare female anomaly of a patent pouch opening from the pelvic cavity floor to the labia majora. It is the female equivalent of a patent processes vaginalis in males. It develops alongside the gubernaculum when the ovaries descend during the development of the urinary and reproductive organs. It can form cysts or a hydrocele and cause various complications [1].
Here, we present a case of a Nuck canal cyst (NCC) associated with endometriosis that was difficult to diagnose using conventional haematoxylin and eosin (HE) staining due to severe degeneration and the presence of surrounding inflammatory tissue. We discuss the diagnostic usefulness of immunohistochemistry (IHC) and provide a brief review of the relevant literature.
Case report
A 42-year-old woman presented to her local practicing doctor with right groin discomfort that had been present for 5 years. She had never experienced any groin pain or periodic inguinal swelling or shrinking in relation to her menstrual cycle. An ultrasound scan (US) revealed a multicystic lesion in the right inguinal canal, indicating an inguinal hernia and raising the possibility of NCC. She then declined the surgical intervention recommended by the referring physician. One year later, the progression of the swelling of the inguinal lesion prompted her to seek medical attention and she was referred to our hospital. US imaging confirmed the cystic lesion in the right groin. A Marcy repair was performed to remove the lesion and close the blind fistula extending from the floor of the pelvic cavity to the right labia majora. The fluid in the fistula was serous and clear.
Macroscopically, the resected specimen showed a blind multicystic tube that extended from the peritoneal cavity into the inguinal canal (Fig. 1a). A small dark brown nodule measuring ~4 × 3 mm protruded from the cyst wall into the lumen (Fig. 1b). Histologically, the canal lumen was lined with a single layer of calretinin-positive mesothelial cells (Fig. 2a). In contrast, the surface of the protruding nodule was erosive, lacking covering cell layer (Fig. 2b). At first glance under low-power, the nodule was considered to be granulation tissue (Fig. 2b). However, closer examination under high-power observation revealed multiple clusters of hemosiderin-laden macrophages scattered throughout the granulation tissue (Fig. 2c). In addition, scrutiny of the entire specimen under high-power view also showed a few inconspicuous glands which, due to severe degeneration, could not be characterized with certainty by HE staining (Fig. 2d). Nonetheless, the haemosiderin deposition and the presence of vestigial glands raised the possibility of endometriosis.
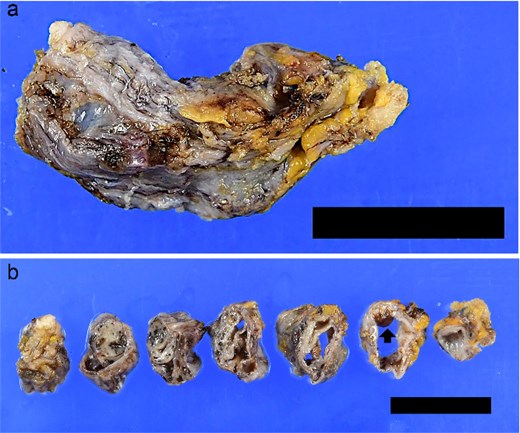
Macroscopic view of the resected specimen. (a) The resected tissue showed a sheath-like appearance. (b) On cross-section, the lesion consisted of branched canal with partial dilatation. A small dark-brownish mural protuberance (arrow) was noted. (a and b) bar = 2 cm.
To ascertain whether this ‘granulation tissue’ was indeed endometriosis, immunohistochemical staining was performed using the CD10 antibody, which recognizes the background stromal cells of endometriosis [2, 3]. The stromal cells within the granulation tissue were stained with CD10 (Fig. 2e). In addition, the nuclei of the degenerated glands embedded in the granulation tissue were positive for oestrogen receptor (Fig. 2f). These findings strongly suggested that this ‘granulation tissue’ was a residual endometriosis lesion. We concluded that this was a case of NCC with endometriosis.
![Microscopic findings of the resected specimen. (a) A smooth luminal surface was covered with calretinin-positive monolayer cells (left half of the figure), whereas the surface of mural protruding nodule (right lower of the figure [corresponds to the ‘arrow’ part in Fig. 1b]) lacked covering cell layer (immunohistochemistry with calretinin ×100). (b) At first glance in low-power view, mural protruding nodule seemed like a granulation tissue (HE, ×40). (c) Dense infiltrates of hemosiderin-laden macrophages were seen across the granulation tissue (HE, ×400). (d) A few degenerated, inconspicuous glands with uncertain characteristics were observed (HE, ×400). (e) Some stromal cells around gland-like cell arrangement in the ‘granulation tissue’ were CD10 positive (×400). (f) The nuclei of these degenerated glands were positive for oestrogen receptor (×400).](https://oupdevcdn.silverchair-staging.com/oup/backfile/Content_public/Journal/jscr/2025/8/10.1093_jscr_rjaf540/1/m_rjaf540f2.jpeg?Expires=1773824596&Signature=SpAZBRWPjOEdF3ggLHE7Iqv0BIKeVMLMP6RCJgV~N1PDqVRV1Uep3G3QWhiLyVStrMOL1XXoWF~nSXaXg7ip-AQqCOVFtydpmkYbhX8g4Kk~4XAOW5wRZiovz7qFGW3lMVS3350OboANRtEmQmqohZ~urx328GwCJ4rHs7L8nCgHgDYxSpFPhJS2ZjFtgjGJ70aJxWjYMhx4mt3szflYudx3KtLAsMtKVmTy5jI~8bP-y7Fp~-E3o~rgX-N4QOWjgHJ6j2sL4H2DHMOFHfQosd3wl-MCq1POeV54QaHKx-EZXoXbdO7uttQnz50-8KZXBqmW4Kg~zxl6kUV0BP1NWQ__&Key-Pair-Id=APKAIYYTVHKX7JZB5EAA)
Microscopic findings of the resected specimen. (a) A smooth luminal surface was covered with calretinin-positive monolayer cells (left half of the figure), whereas the surface of mural protruding nodule (right lower of the figure [corresponds to the ‘arrow’ part in Fig. 1b]) lacked covering cell layer (immunohistochemistry with calretinin ×100). (b) At first glance in low-power view, mural protruding nodule seemed like a granulation tissue (HE, ×40). (c) Dense infiltrates of hemosiderin-laden macrophages were seen across the granulation tissue (HE, ×400). (d) A few degenerated, inconspicuous glands with uncertain characteristics were observed (HE, ×400). (e) Some stromal cells around gland-like cell arrangement in the ‘granulation tissue’ were CD10 positive (×400). (f) The nuclei of these degenerated glands were positive for oestrogen receptor (×400).
Discussion
NCC is a female genitourinary malformation in which a patent peritoneal pouch extends from the floor of the pelvic cavity into the labia majora via the inguinal canal. It is caused by the failure of the pouch attached to the gubernaculum to obliterate during the development of the urogenital organs, when it descends with the ovaries.
The pouch usually closes in early infancy, but it can remain open until adolescence or adulthood. This can be asymptomatic or cause various symptoms, ranging from inguinal/labial swelling to serious complications.
NCC is rare [4]. In a review of surgical case series for inguinal hernias in females, NCC was found in 0.76% of cases [5]. However, cases of NCC may go unnoticed by patients because the symptoms are minimal or it may be mis-diagnosed and treated as conventional inguinal hernia.
In our case, the NCC was located in the right groin area. NCCs tend to occur on the right side. One study found that 82.4% of NCC cases occurred on the right side [1]. Interestingly, the male counterpart of NCC, hydrocele testis, also shows a statistically significant predilection for the right side (56.7% in boys under 15 and 64.3% in older males) [6]. In males, the left testis descends earlier than the right and the left processus vaginalis closes earlier. This may explain why right-sided hydrocele testis increases with age.
In our case, the NCC was associated with endometriosis. The incidence of endometriosis in NCC cases is reported to be 0.3%–0.6% of all endometriosis cases [7]. Interestingly, there is a reported case of monozygotic twin sisters who both had right-sided NCC and subsequently developed endometriosis in the NCC almost simultaneously (within a 1-year interval) [8]. These cases suggest that genetic factor(s) may play a role in the occurrence of NCC and endometriosis.
When the endometriosis is obscured by degeneration or masked by post-inflammatory changes, it can be difficult to discern with conventional HE staining alone. With the aid of IHC, however, we were able to decipher endometriosis buried within the granulation tissue.
NCC can sometimes present with mild symptoms such as inguinal/genital discomfort or swelling. However, it can occasionally cause more serious complications such as incarcerated ovarian herniation [9], ectopic pregnancy [10], and inguinal metastasis from ovarian cancer [11]. In addition, NCC associated with endometriosis can be the site of origin for clear cell carcinoma [12], endometrioid carcinoma [13], and endometrial stromal sarcoma [14], although these are extremely rare events.
Bearing in mind the risks of these complications, the possibility of NCC should be actively considered in women presenting with inguinal or labial swelling. If NCC is suspected, surgical removal should be considered to both remove the lesion and eliminate the potential risk of various complications.
When associated with endometriosis, there is a risk of secondary malignancies. If endometriosis is suspected, IHC for CD10 and oestrogen receptor should be used actively to confirm the diagnosis.
Conflict of interest statement
None to be declared.
Funding
No sources of funding to be disclosed.



