-
PDF
- Split View
-
Views
-
Cite
Cite
Rehab M Al Hamoud, Khalid Aljohani, Abdullah S Al-Darwish, Bushr Mrad, Adult right-sided strangulated diaphragmatic hernia with history of open nephrectomy: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 8, August 2025, rjaf473, https://doi.org/10.1093/jscr/rjaf473
Close - Share Icon Share
Abstract
We present a case involving a 76-year-old man who developed a strangulated diaphragmatic hernia 14 years after undergoing an open right nephrectomy for renal cell carcinoma. The patient presented with lower abdominal pain, vomiting, and constipation. Imaging studies revealed an obstructed segment of the bowel herniating through a defect in the posterior right hemidiaphragm, along with signs of strangulation. An urgent laparotomy was performed, during which a right hemicolectomy was conducted. Despite experiencing hemodynamic instability, the patient eventually underwent an ileocolic anastomosis and a primary repair of the diaphragmatic defect. He made a rapid recovery and was discharged in stable condition. This case report aims to raise awareness about the risk of inadvertent diaphragmatic injury during open nephrectomy. It also emphasizes the importance of timely diagnosis and appropriate surgical management to prevent complications and improve patient outcomes.
Introduction
Inadvertent diaphragmatic injury can occur during open flank surgery for renal or adrenal disease, leading to potential complications. We present a case of a 76-year-old man who developed a strangulated diaphragmatic hernia 14 years after an open right nephrectomy for renal cell carcinoma.
Case report
A 76-year-old man presented to the emergency department with a 3-day history of lower abdominal pain. The pain began gradually and progressively worsened. It was dull in nature and had no specific aggravating or relieving factors. Additionally, he experienced nausea, along with two episodes of vomiting gastric contents, and constipation. He denied having fever, weight loss, rectal bleeding, or respiratory symptoms. Prior to this acute illness, he had been in good health, with a history of hypertension. Fourteen years ago, he underwent a curative open right nephrectomy for renal cell carcinoma.
Upon admission, the patient appeared well, alert, and oriented. His pulse rate was 80 beats per minute, and his blood pressure was 150/82 mmHg. The respiratory rate was 16 breaths per minute, with an oxygen saturation of 94% on room air. The patient exhibited no signs of respiratory distress.
Physical examination revealed that the abdomen was soft, with mild tenderness noted in the right lower quadrant. A digital rectal examination was unremarkable. Blood tests upon presentation showed the following results: hemoglobin 14.2 g/dl, white blood cell count 6000 cells/mm3, platelets 264 × 109/l, sodium 142 mmol/l, potassium 3.82 mmol/l, urea 6.5 mmol/l, creatinine 103 mmol/l/l, alkaline phosphatase 57 U/l, alanine transferase 7.3 U/l, bilirubin 9.1 mmol/l, and albumin 42 g/l. An electrocardiogram indicated a normal sinus rhythm.
The patient was initially resuscitated with intravenous fluids. An urgent abdominal computed tomography (CT) scan was performed, revealing a herniated and obstructed segment of large bowel loops with mesenteric fat at the hepatic flexure, likely through the posterior right hemidiaphragm (Fig. 1). The scan showed a proximally dilated cecum and ascending colon, with a transitional zone observed at the neck of the hernia, leading to a distally collapsed colon. Additionally, there was an area suspicious for pneumatosis intestinalis within the obstructed bowel segment, along with adjacent fat stranding and free fluid—findings that raised concerns for strangulation or early ischemia. The scan also indicated a right-sided pleural effusion and adjacent atelectasis (Fig. 2).
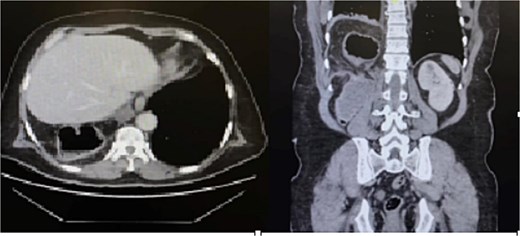
CT scan of the abdomen revealed a herniated obstructed segment of large bowel loops and mesenteric fat at the hepatic flexure, likely through the posterior right hemidiaphragm.
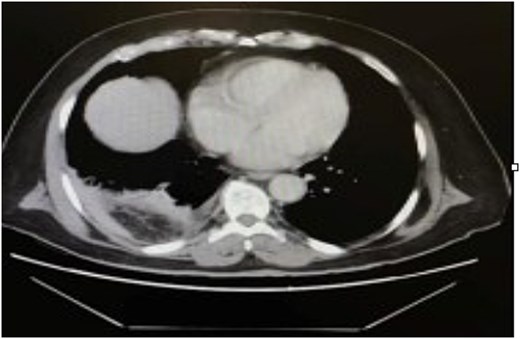
CT scan of the thorax revealed a right-sided pleural effusion and adjacent atelectasis.
The patient was taken for an immediate laparotomy. During the procedure, the cecum and ascending colon were found to be herniated through a defect in the posterior right hemidiaphragm, accompanied by severe adhesions. The bowel appeared dusky with multiple serosal tears, necessitating a right hemicolectomy. After the resection, the patient became hypotensive, with blood pressure dropping to 50/20 mmHg. Fluid resuscitation was initiated, followed by inotropic support as needed by the anesthesia team. The patient was then transferred to the intensive care unit after the abdomen was temporarily closed for hemodynamic stability.
After 48 h, the patient was taken back to the operating room for an ileocolic anastomosis and a primary repair of the diaphragmatic defect. Postoperatively, the patient was transferred to the intensive care unit for continued ventilation and treatment. However, he rapidly recovered, was extubated 24 h later, and was shifted to the surgical floor in stable condition.
Discussion
Diaphragmatic injury is an uncommon but serious complication of open flank surgeries such as nephrectomy or adrenalectomy. These injuries are typically recognized intraoperatively and are repaired with primary suturing and concurrent evacuation of pleural air to prevent postoperative complications [1]. However, when such injuries go unnoticed, they may remain clinically silent for years and eventually present as strangulated diaphragmatic hernias. This delayed manifestation can result in bowel incarceration, ischemia, and even life-threatening cardiopulmonary compromise [2].
Right-sided diaphragmatic hernias in adults are particularly rare due to the protective effect of the liver, and their symptoms can be nonspecific. Patients may present with dyspnea, chest pain, abdominal discomfort, postprandial fullness, nausea, vomiting, or signs of bowel obstruction [3]. In some cases, pleural effusion may be the initial manifestation, especially when ischemic bowel migrates into the thoracic cavity [2]. In our case, the patient presented primarily with gastrointestinal symptoms—lower abdominal pain and vomiting—without respiratory complaints, making the diagnosis more challenging.
The sensitivity of chest radiography in detecting diaphragmatic defects is relatively low, especially on the right side. Therefore, contrast-enhanced CT is considered the gold standard for diagnosis, as it provides detailed anatomical visualization of the diaphragm and any herniated abdominal contents [4, 5]. CT imaging in our case allowed for rapid and accurate diagnosis of a right-sided strangulated diaphragmatic hernia, prompting immediate surgical intervention.
Timely recognition and surgical repair are essential to prevent serious complications such as strangulated bowel, which requires emergency intervention. In cases where diaphragmatic injuries are identified late, surgical treatment via laparotomy or thoracotomy remains the only curative approach [3]. Our patient underwent an urgent laparotomy, which proved lifesaving.
Although rare, diaphragmatic injury during nephrectomy must remain a consideration, especially in patients presenting postoperatively with unexplained abdominal or respiratory symptoms. Routine intraoperative inspection of the diaphragm and high clinical suspicion in postoperative follow-up are crucial to preventing delayed diagnosis and reducing associated morbidity and mortality [1, 3].
Conflict of interest statement
None declared.
Funding
None declared.



