-
PDF
- Split View
-
Views
-
Cite
Cite
Anas Derkaoui, Tarik Deflaoui, Intissar Aissi, Mohammed Hassani, Soufiane Karmouni, Abdelali Guellil, Rachid Jabi, Mohammed Bouziane, Transverse colon perforation secondary to necrotizing pancreatitis: a rare and life-threatening complication, Journal of Surgical Case Reports, Volume 2025, Issue 7, July 2025, rjaf567, https://doi.org/10.1093/jscr/rjaf567
Close - Share Icon Share
Abstract
A 43-year-old man with prior alcohol use and chronic smoking presented with abdominal pain, melena, and fever, on a background of subacute epigastric pain. CT imaging revealed Balthazar E necrotizing pancreatitis with transverse colonic thickening and signs of sealed perforation. Emergency laparotomy uncovered purulent peritonitis and a large perforation of the mid-transverse colon adherent to necrotic pancreatic tissue. A right extended hemicolectomy with double stoma and retroperitoneal lavage was performed. Histopathology confirmed colonic wall necrosis without malignancy. This case illustrates a rare and life-threatening colonic complication of necrotizing pancreatitis. It emphasizes the importance of early suspicion, cross-sectional imaging, and timely surgical management in reducing morbidity and mortality in such complex settings.
Introduction
Necrotizing pancreatitis is a severe complication of acute pancreatitis that can extend to adjacent organs, including the gastrointestinal tract. Colonic complications, although rare, are associated with significant morbidity and mortality [1, 2]. These include ischemia, fistulas, and, less commonly, perforation. The transverse colon is particularly vulnerable due to its proximity to the pancreas and its watershed blood supply. This report presents a rare case of transverse colon perforation secondary to necrotizing pancreatitis, managed surgically with favorable outcome.
Necrotizing pancreatitis is a severe complication of acute pancreatitis that can extend to adjacent organs, including the gastrointestinal tract. Colonic complications, although rare, are associated with significant morbidity and mortality [1, 2]. Specifically, studies indicate that colonic involvement occurs in a small but significant percentage of patients with necrotizing pancreatitis, often leading to severe outcomes such as requiring colectomy [3]. These include ischemia, fistulas, and, less commonly, perforation. The incidence of gastrointestinal perforations and fistulas in this context, while low, underscores the severity of pancreatic necrosis extending to adjacent structures [4]. The transverse colon is particularly vulnerable due to its proximity to the pancreas and its watershed blood supply. This report presents a rare case of transverse colon perforation secondary to necrotizing pancreatitis, managed surgically with favorable outcome.
Case presentation
A 43-year-old man, with a 30-pack-year smoking history and remote alcohol consumption (abstinent for 1 year), presented with worsening abdominal pain and low-grade melena over 3 days, following 2 months of intermittent epigastric discomfort. Upon deterioration, the patient presented to our emergency department with fever, anorexia, and generalized abdominal pain.
On examination, he was stable, afebrile, with epigastric defense and generalized tenderness. Digital rectal examination revealed traces of melena. Laboratory tests revealed leukopenia (3700/mm3), anemia (Hb 8.4 g/dl), elevated CRP (112 mg/l), procalcitonin (18 ng/ml), hypoalbuminemia (29 g/l), and elevated creatinine (9.6 mg/l). Liver enzymes and electrolytes were within acceptable ranges. Based on admission data, the patient’s estimated APACHE II score was at least 7, indicating a significant severity.
A contrast-enhanced abdominal CT showed Balthazar E pancreatitis with peripancreatic necrosis, thickening of the transverse colon and first jejunal loop, and sealed colonic perforation. Perisplenic and perihepatic fluid collections were noted, with no free air (Figs 1 and 2).
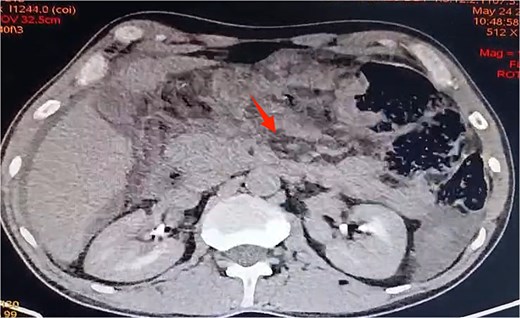
Axial view of contrast-enhanced abdominal CT scan revealing Balthazar E pancreatitis with peripancreatic necrosis.
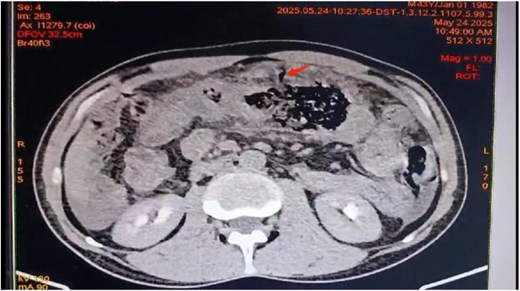
Axial view of contrast-enhanced abdominal CT scan revealing transverse colon wall thickening and a sealed transverse colon perforation.
Emergency laparotomy revealed a large sealed perforation of the mid-transverse colon adherent to the first jejunal loop and omentum, purulent peritoneal effusion, and a fibrotic, inflamed duodeno-pancreatic block. The remainder of the gastrointestinal tract was unremarkable. A right extended hemicolectomy with double stoma, retroperitoneal lavage, and multiple drainages was performed (Figs 3–6).
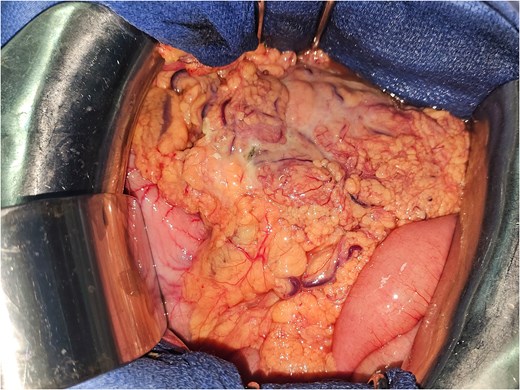
Intraoperative image showing the thickened and infiltrated appearance of the transverse colon with a perforation contained by the omentum and the first ileal loop.
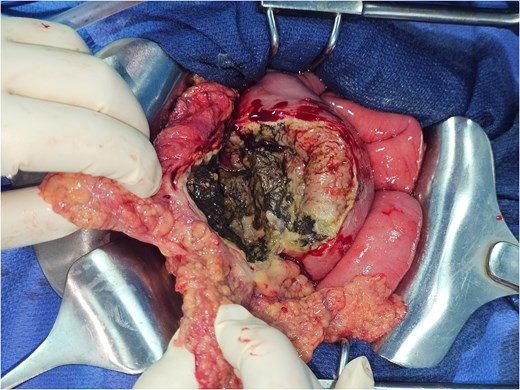
Intraoperative image showing the perforation of the middle third of the transverse colon.
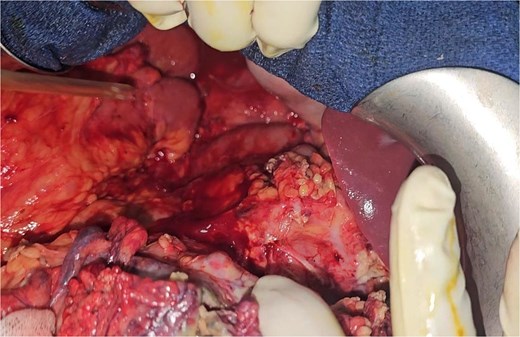
Intraoperative image of the lesser sac (or omental bursa) showing pancreatic infiltration with necrosis collections (or necrotic fluid collections).

Image of the surgical specimen of a right hemicolectomy showing the perforation.
The postoperative course was favorable under broad-spectrum antibiotics and intensive care support. Histology confirmed colonic wall necrosis and transmural inflammation without malignancy. The patient will be scheduled for a cholecystectomy (given the pancreatitis is gallstone-related) and a restoration of continuity in 3 months.
Discussion
Gastrointestinal involvement in necrotizing pancreatitis is rare but potentially lethal. Colonic complications are reported to occur with an incidence ranging from 10% to 19% in patients with necrotizing pancreatitis, often involving the splenic flexure or transverse colon [3]. A nationwide prospective cohort study further highlights that perforations and fistulas of the gastrointestinal tract, including the colon, represent serious but less frequent complications within the spectrum of necrotizing pancreatitis [4]. Mechanisms include direct enzymatic injury, ischemia, and inflammatory spread from retroperitoneal necrosis [5].
The transverse colon lies in close anatomical proximity to the pancreas and is particularly susceptible due to dual vulnerabilities: its position adjacent to the pancreatic tail and its relative hypovascularity at the watershed Griffiths’ point [6, 7]. In our case, the inflammatory spread and pressure from necrotic collections likely caused progressive wall weakening leading to sealed perforation.
The clinical presentation of colonic involvement is subtle, often masked by signs of pancreatitis. Gastrointestinal bleeding, as observed in our patient, is an uncommon but crucial red flag [8, 9]. Imaging with contrast-enhanced CT is the most sensitive modality, revealing mural thickening, fat stranding, pericolonic fluid, and sealed defects [10].
Management strategies depend on the timing and severity of the perforation. While open surgical resection with fecal diversion, as performed in our case, remains a critical approach in acute settings with diffuse peritonitis and overt perforation, primary anastomosis is generally contraindicated due to the hostile, inflamed field and immunocompromised status of patients. Our approach, combining resection with double stoma and retroperitoneal lavage, aligns with damage-control principles advocated in such settings [11, 12]. However, contemporary literature also explores less invasive options for managing severe necrotizing pancreatitis with colonic necrosis. For instance, video-assisted retroperitoneal debridement has been successfully employed in some cases of severe pancreatitis complicated by colonic perforation, particularly when managing localized necrosis and infections [13]. For cases requiring extensive colonic resection due to severe complications, subtotal colectomy has also been reported [14].
Mortality remains high if diagnosis or surgery is delayed. Reported mortality from colonic perforation in necrotizing pancreatitis reaches up to 50% in some series [15]. Favorable outcomes depend on early recognition, prompt surgical intervention, and multidisciplinary care, including critical care and nutritional support [16, 17].
Conclusion
Colonic perforation is a rare but serious complication of necrotizing pancreatitis, often masked by nonspecific symptoms and delayed diagnosis. The transverse colon, due to its anatomical proximity and vascular vulnerability, may be affected by local inflammation and ischemia. This case underscores the importance of high clinical suspicion, thorough imaging, and prompt surgical management. A multidisciplinary approach combining resection, fecal diversion, and retroperitoneal drainage can lead to favorable outcomes even in critically ill patients. Early recognition and aggressive intervention remain the cornerstones of treatment to reduce morbidity and mortality in such complex presentations.
Conflict of interest statement
None declared.
Funding
None declared.



