-
PDF
- Split View
-
Views
-
Cite
Cite
AbdulRahman M Alkabli, Mohammed Basem Beyari, Faisal AlOmri, Ali Alzahrani, Laparoscopic treatment for a rare case of giant spleen with splenic arteriovenous fistula and giant vein aneurysm: multidisciplinary management and case report, Journal of Surgical Case Reports, Volume 2025, Issue 7, July 2025, rjaf531, https://doi.org/10.1093/jscr/rjaf531
Close - Share Icon Share
Abstract
Splenic arteriovenous fistula (SAVF) is a rare vascular condition characterized by an abnormal connection between the splenic artery and vein, often leading to complications such as portal hypertension. While uncommon, SAVFs can arise from trauma, inflammatory diseases, or idiopathically. They frequently coexist with splenic artery aneurysms, complicating diagnosis and management. Advances in imaging, particularly computed tomography angiography, have significantly improved detection, enabling earlier intervention. If left untreated, SAVFs can result in severe complications, including gastrointestinal bleeding and non-cirrhotic portal hypertension. Early recognition is crucial for preventing life-threatening outcomes and optimizing treatment. The laparoscopic approach has gained attention as a less invasive alternative. However, laparoscopic management presents significant technical challenges due to the complex vascular anatomy, risk of excessive bleeding, and difficulty in accessing the splenic hilum.
Introduction
Splenic arteriovenous fistula (SAVF) is an unusual vascular condition that involves an abnormal connection between the splenic artery and vein, often leading to complications such as portal hypertension. Although uncommon, SAVFs have been observed to occur after events like trauma, inflammatory diseases, or sometimes without any apparent cause, which is termed “idiopathic” [1, 2]. The condition often coexists with splenic artery aneurysms (SAAs), adding complexity to its clinical presentation and management [3, 4]. The condition is challenging because it often goes undetected until complications arise, making prompt recognition essential for effective management and improved outcomes [1–3].
Diagnostic imaging plays a crucial role in allowing for visualization of the vascular connection and assessment of the resulting portal hypertension. In cases with significant vascular anomalies, computed tomography angiography can reveal early filling of the splenic vein from the splenic artery, indicating the presence of a fistula [2–6].
Management of SAVF is individualized, depending on the patient’s symptoms and the size and location of the fistula. Traditionally, open surgery, including splenectomy, was the preferred approach and remains effective for many cases [4, 5]. Ultimately, treatment is selected based on the patient’s anatomy and overall health, with recent case reports highlighting the effectiveness of both surgical and endovascular techniques in achieving positive outcomes [3–5, 7].
Case presentation
A 36-year-old female medically free Gravida Ten, presented to the emergency department with copious hematemesis and left upper quadrant abdominal pain that started 22 days prior to presentation. She denied fever, chills, night sweats, weight loss, and chest pain. No family history of medical illness. Non-smoker and not alcoholic. Upon arrival the patient vitally stable afebrile. The abdomen was soft, lax, with tenderness at the left quadrant, mildly distended, with palpable spleen on the left side of the abdomen.
A computed tomography (CT) scan was obtained as part of the patient’s investigation plan, for which it revealed: no active bleeding. There was a distal SAA measuring 1.9 cm (Fig. 1c) with focal arteriovenous (AV) fistula with the distal splenic vein causing shunting of the flow with resultant severe aneurysmal dilatation of the splenic vein measures 3.4 × 9 × 4 cm (Fig. 1a–c). There were signs of portal hypertension seen as dilated portal vein measuring 2.8 cm (Fig. 2a and b) enlarged spleen measuring 20 cm. Other than that, the remaining of the CT was unremarkable.
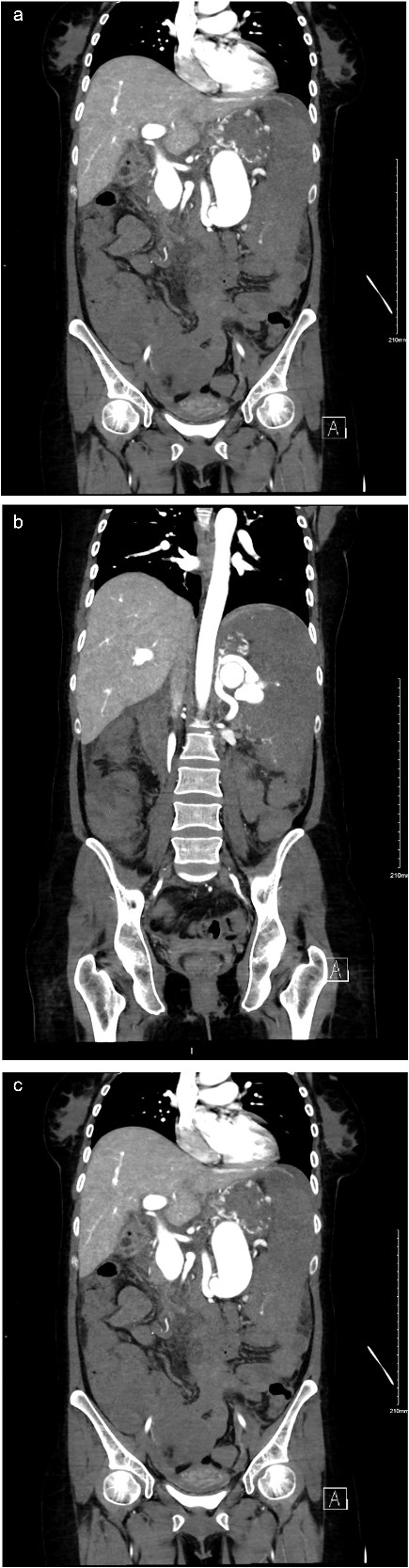
(a) Coronal view of enhanced CT of abdomen and pelvis showing dilated splenic vein lateral to the artery. (b) Coronal view of enhanced CT of abdomen and pelvis showing dilated splenic vein causing portal hypertension. (c) Coronal view of enhanced CT of abdomen and pelvis delayed imaging showing the AV fistula at the hilum.
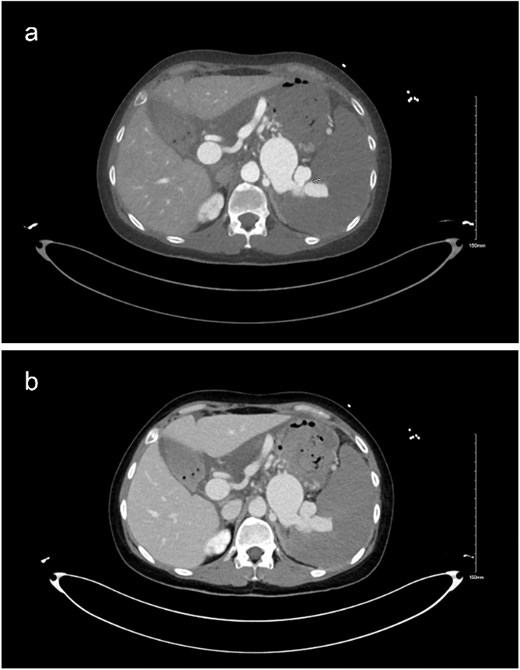
(a and b) Delayed imaging CT of the abdomen and pelvis in axial view, showing the distended splenic vein and AV fistula at the hilum.
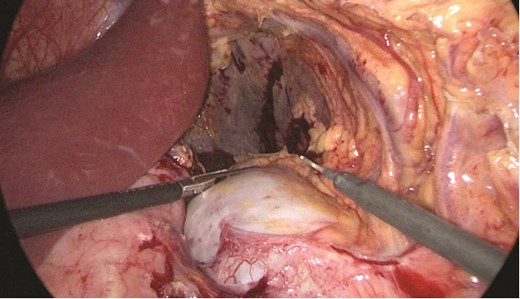
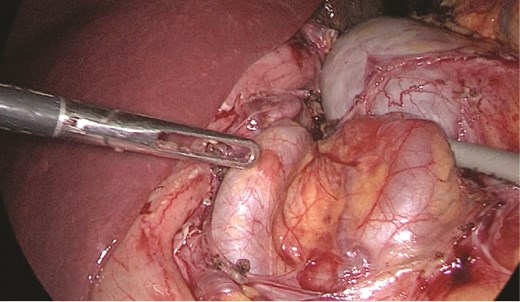
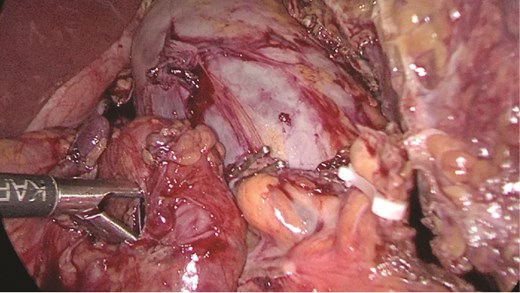
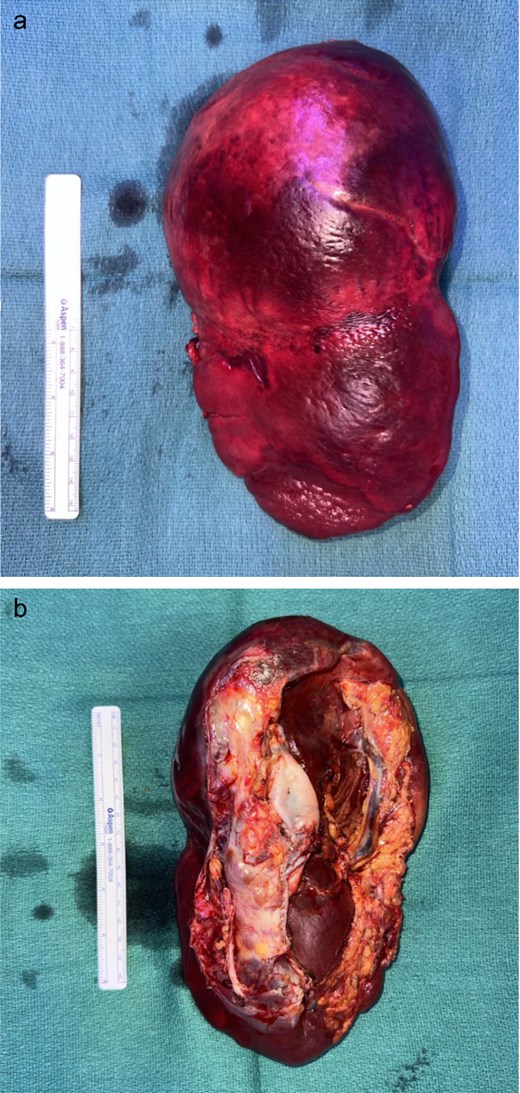
Multidisciplinary discussion was held to evaluate the most appropriate course of action for the patent condition, and the consensus was reached to pursue embolization as a first intervention. Embolization was performed by interventional radiology with no complications post-procedure, and the patient was optimized prior to her procedure. Patient was taken to the operating room in stable conditions. The spleen was enlarged around 20 cm. Inferiorly, the omentum and part of the transverse colon was attached to the spleen (Fig. 3), so we freed the omentum from the splenic tissue. The dissection continued until reaching short gastric vessels and entering the lesser sac (Fig. 4). Once the lesser sac was entered, the splenic vessels were identified (Figs 5 and 6), the splenic vein was hugely dilated with multiple collateral branching vessels at the hilum. Gaining posterior mobilization of the vein was challenging. The splenic artery was tortuous from the insertion around itself (Fig. 7). After complete mobilization of the fundus, we elected to divide each vessel starting with the splenic artery so we can achieve full mobilization of the vein (Fig. 9). After controlling the splenic artery, the splenic vein was dissected proximal to the splenic hilum (Fig. 8). It was hugely dilated and its wall is thickened secondary to AV fistula. It was difficult to achieve circumferential dissection, so we decided at that moment to convert to laparotomy to complete ligating the vein and to retrieve the specimen (Fig. 10a and b).

The spleen inferiorly, attached to it the mesentery and the transverse colon.
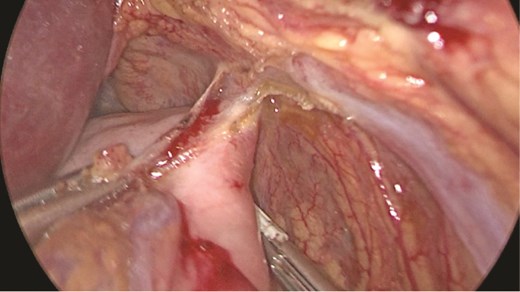
Stomach attached to the medial border of the spleen. Short gastric vessels.
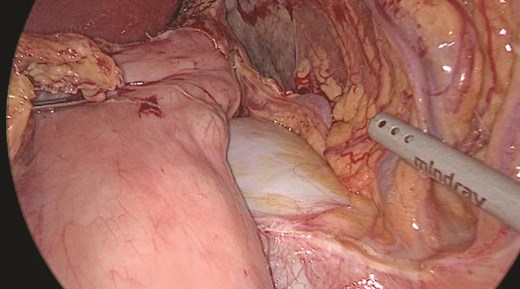
Anterior portion of the splenic vein seen posterior to the stomach.
Anterior portion of the splenic vein seen posterior to the stomach.
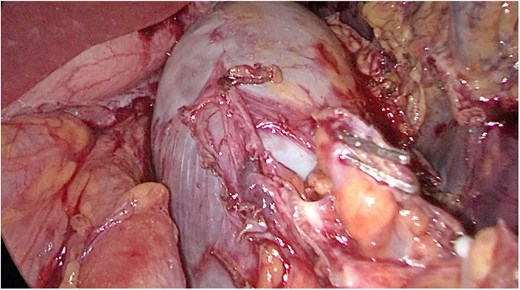
Splenic vein mobilized from the side. Clips seen on branches of the vein.
Discussion
Cirrhosis is considered the most common cause of portal hypertension. However, non-cirrhotic portal hypertension is ought to be an important clinical entity for physicians to recognize. The surgeon should consider splanchnic AV fistulas in the differential for non-cirrhotic portal hypertension [8, 9]. Imaging should be obtained to assess these conditions to avoid delays in diagnosis and management. In our case, the patient initially underwent a transcatheter arterial embolization trans arterial embolization. There was significant high flow from the superior mesenteric artery and arteriovenous fistula with aneurysmal dilatation and significantly enlarged splenic veins with high flow to the portal vein. The proximal splenic artery was embolized utilizing 12 mm Aplatzer Plug. Three days after the procedure, the patient was prepared for definitive management. We believe that early intervention is of greatest importance for splenic AV fistula because of the serious late complications that could happen if left untreated [10]. In general, laparoscopic splenectomy was not recommended for patients with organs >20 cm. Guidelines published by the European Association of Endoscopic Surgery also suggest that open or hand assisted surgery should be considered if spleen size >20 cm [11, 12]. Nevertheless, successful laparoscopic excision of spleens >20 cm has been reported by other authors [13–15]. Additionally, adhesions that can obscure anatomical landmarks and make dissection more difficult. Surgeon experience plays a pivotal role in overcoming these challenges. BMI has been utilized as a measurable parameter to assess the impact of body habitus on surgical planning and complications.
Conclusion
This case highlights the complex management of a patient with splenic AV fistula. Laparoscopic approach is a viable and effective option splenectomy, despite its technical challenges. Careful patient selection is crucial for safe procedures. Further studies are essential to expand the topic of laparoscopic approach to large spleens.
Author contributions
AbdulRahman M. Alkabli (Conceptualization, Data curation, Investigation, Validation, Writing, and Editing final draft). Ali Alzahrani (Supervision, Validation), Mohammed Basem Beyari (Data curation, Writing). Faisal Al Omri (Writing, Curation, Investigation).
Conflict of interest statement
None declared.
Funding
Not applicable; no funding was required.



