-
PDF
- Split View
-
Views
-
Cite
Cite
Nader Alharbi, Areej Alqarzie, Mohammed Bajahzer, Faris Alnosayan, Our approach to endoscopic septoplasty: Intra Nasal Endoscopic Septoplasty with NOSE score analysis, Journal of Surgical Case Reports, Volume 2025, Issue 6, June 2025, rjaf453, https://doi.org/10.1093/jscr/rjaf453
Close - Share Icon Share
Abstract
Deviation of the nasal septum is a common cause of nose obstruction, often requires surgical management with septoplasty, which can involve significant tissue manipulation and extended recovery time. This case series demonstrates the use of the Intra Nasal Endoscopic Septoplasty (INES) technique, a minimally invasive approach, for managing unilateral septal deviations. Six patients presenting with nasal obstruction underwent INES, with outcomes assessed pre- and postoperatively using the Nasal Obstruction Symptom Evaluation (NOSE) scale. Follow-up over 6 months evaluated changes in NOSE scores, complication rates, and patient satisfaction. Postoperative results demonstrated significant symptom improvement, with relief ranging from 84.6% to 100%. The cumulative NOSE score showed a statistically significant reduction (P = 0.034), though individual NOSE criteria did not reveal significant changes. The procedure yielded high patient satisfaction in a short period and no major complications. Larger studies are necessary to confirm these results and further explore the long-term efficacy of INES.
Introduction
In otolaryngology, septoplasty is a surgery used to treat deviated nasal septum problems, which can lead to severe breathing difficulties, persistent sinusitis, and a decreased quality of life for patients [1]. The nasal septum has been extensively manipulated during septoplasty procedures, which frequently call for hemi-transfixion and Killian’s incisions, the formation of unilateral or bilateral mucosal flaps, and significant cartilage shaping [2, 3]. Despite their effectiveness, these traditional methods have the potential to cause long-term structural problems, avoidable complications, and longer periods of recovery.
An Intra Nasal Endoscopic Septoplasty (INES) is a method created especially for selected unilateral septum deviation presented in this article. In contrast to conventional techniques, this method involves single-sided mucosal flap elevation and targeted correction of the deviated septum only. By minimizing tissue disruption, preserving more of the nasal structures’ natural morphology, and reducing surgical time, this approach may lessen surgical injury and improve patients’ overall recovery.
This study’s main goal is to evaluate the effectiveness and efficiency of our approach using a case series involving six patients followed up over 6 months. To quantify pre and post-operative outcomes objectively, we employ the Nasal Obstruction Symptom Evaluation (NOSE) scale, a validated disease-specific quality-of-life tool for nasal obstruction [4]. The NOSE score is a standardized indicator of the severity of symptoms of nasal obstruction and the outcome of surgery. It is composed of five measures that evaluate nasal congestion, obstruction, breathing difficulties, sleep, and activity. We also assess other outcome indicators, such as recovery time, complication rates, and patient satisfaction.
Because this method is less invasive and preserves the integrity of the septum on the non-deviated side, we believe it could be especially helpful for selected cases of septal deviation. By thoroughly examining these elements, we intend to offer valuable insight on the possible advantages and negative aspects of our technique. The results of this study may have major implications for surgical practice, which could result in better patient outcomes, lower healthcare costs, and a higher standard of life quality for patients undergoing septoplasty.
Methods
This case series evaluated patients who underwent intranasal endoscopic septoplasty between January 1, 2024, and October 30, 2024. All patients presented with symptomatic nasal obstruction due to a deviated nasal septum and underwent a comprehensive preoperative assessment, including a detailed history, physical examination, and nasal endoscopy. Inclusion criteria were limited to patients with unilateral nasal obstruction caused by a unilateral septal deviation classified as type 5 or type 6, according to Mladina’s classification, and who were undergoing septoplasty as the sole procedure without any additional interventions.
The severity of nasal obstruction was assessed in all patients using the NOSE questionnaire, a validated tool for measuring nasal obstruction. The NOSE questionnaire evaluates five items related to nasal breathing difficulties, with responses graded on a Likert scale from 0 (no problem) to 4 (severe problem). The total score is then converted to a scale of 0–100, with higher scores reflecting greater symptom severity.
Postoperatively, patients were followed up and re-evaluated at multiple visits over 6 months period, during which the NOSE questionnaire was re-administered to assess symptom improvement. Additionally, postoperative complications and patient satisfaction were recorded to provide a comprehensive evaluation of outcomes.
Results
Characteristics of patients
This case series included six patients (mean age 31.33 ± 8.79 years; 66.6% female) with unilateral septal deviations (83.3% right-sided) (Table 1). All patients completed 6 months of follow-ups, with no dropouts or postoperative complications reported.
| N | 6 | |
| Age (SD) | 31.33 | (±8.79) |
| Sex | ||
| Male | 2 | 33.3% |
| Female | 4 | 66.7% |
| Nasal Deviation | ||
| Right Side | 5 | 83.33% |
| Left Side | 1 | 16.67% |
| N | 6 | |
| Age (SD) | 31.33 | (±8.79) |
| Sex | ||
| Male | 2 | 33.3% |
| Female | 4 | 66.7% |
| Nasal Deviation | ||
| Right Side | 5 | 83.33% |
| Left Side | 1 | 16.67% |
Characteristics of patients who underwent the INES, are presented as mean ± standard deviation for continuous data and as frequency and percentage for categorical data.
| N | 6 | |
| Age (SD) | 31.33 | (±8.79) |
| Sex | ||
| Male | 2 | 33.3% |
| Female | 4 | 66.7% |
| Nasal Deviation | ||
| Right Side | 5 | 83.33% |
| Left Side | 1 | 16.67% |
| N | 6 | |
| Age (SD) | 31.33 | (±8.79) |
| Sex | ||
| Male | 2 | 33.3% |
| Female | 4 | 66.7% |
| Nasal Deviation | ||
| Right Side | 5 | 83.33% |
| Left Side | 1 | 16.67% |
Characteristics of patients who underwent the INES, are presented as mean ± standard deviation for continuous data and as frequency and percentage for categorical data.
NOSE score outcomes
The cumulative NOSE scores demonstrated a statistically significant reduction after INES treatment, decreasing from a preoperative median of 85 (range: 35–90) to a postoperative median of 5 (range: 0–10; *P* = 0.034, Wilcoxon signed-rank test). The Cohen’s d effect size of 3.29 (95% CI: 1.15–5.40) indicated a large magnitude of improvement (Table 2).
| Before . | After . | ||||
|---|---|---|---|---|---|
| Range . | Median . | Range . | Median . | P-value . | |
| Nasal congestion of stuffiness | 0–4 | 3.5 | 0–1 | 0 | 0.174 |
| Nasal blockage or obstruction | 2–4 | 3.5 | 0–1 | 0 | 0.057 |
| Trouble breathing through nose | 1–4 | 3.5 | 0–1 | 0 | 0.057 |
| Trouble sleeping | 1–4 | 3 | 0–0 | 0 | 0.058 |
| Unable to get enough air through nose during exercise or exertion | 3–4 | 3.5 | 0–1 | 0 | 0.057 |
| Total score × 5 | 35–90 | 85 | 0–10 | 5 | 0.034 |
| Before . | After . | ||||
|---|---|---|---|---|---|
| Range . | Median . | Range . | Median . | P-value . | |
| Nasal congestion of stuffiness | 0–4 | 3.5 | 0–1 | 0 | 0.174 |
| Nasal blockage or obstruction | 2–4 | 3.5 | 0–1 | 0 | 0.057 |
| Trouble breathing through nose | 1–4 | 3.5 | 0–1 | 0 | 0.057 |
| Trouble sleeping | 1–4 | 3 | 0–0 | 0 | 0.058 |
| Unable to get enough air through nose during exercise or exertion | 3–4 | 3.5 | 0–1 | 0 | 0.057 |
| Total score × 5 | 35–90 | 85 | 0–10 | 5 | 0.034 |
NOSE Scale Scores before and after the INES intervention are presented as the range and median for each question. The Wilcoxon signed rank test was used to compare between the before and after intervention data. The P-value column indicates whether the difference in median scores between pre- and post-treatment is statistically significant (P < 0.05).
| Before . | After . | ||||
|---|---|---|---|---|---|
| Range . | Median . | Range . | Median . | P-value . | |
| Nasal congestion of stuffiness | 0–4 | 3.5 | 0–1 | 0 | 0.174 |
| Nasal blockage or obstruction | 2–4 | 3.5 | 0–1 | 0 | 0.057 |
| Trouble breathing through nose | 1–4 | 3.5 | 0–1 | 0 | 0.057 |
| Trouble sleeping | 1–4 | 3 | 0–0 | 0 | 0.058 |
| Unable to get enough air through nose during exercise or exertion | 3–4 | 3.5 | 0–1 | 0 | 0.057 |
| Total score × 5 | 35–90 | 85 | 0–10 | 5 | 0.034 |
| Before . | After . | ||||
|---|---|---|---|---|---|
| Range . | Median . | Range . | Median . | P-value . | |
| Nasal congestion of stuffiness | 0–4 | 3.5 | 0–1 | 0 | 0.174 |
| Nasal blockage or obstruction | 2–4 | 3.5 | 0–1 | 0 | 0.057 |
| Trouble breathing through nose | 1–4 | 3.5 | 0–1 | 0 | 0.057 |
| Trouble sleeping | 1–4 | 3 | 0–0 | 0 | 0.058 |
| Unable to get enough air through nose during exercise or exertion | 3–4 | 3.5 | 0–1 | 0 | 0.057 |
| Total score × 5 | 35–90 | 85 | 0–10 | 5 | 0.034 |
NOSE Scale Scores before and after the INES intervention are presented as the range and median for each question. The Wilcoxon signed rank test was used to compare between the before and after intervention data. The P-value column indicates whether the difference in median scores between pre- and post-treatment is statistically significant (P < 0.05).
At the individual patient level, symptom improvement ranged from 84.6% to 100%, with an average reduction of 94.5% in NOSE scores (Table 3). Two patients achieved complete resolution of symptoms (100% improvement), while the remaining four showed marked reductions (84.6%–94.4%). Subjective improvements were reported within 1–4 weeks postoperatively (mean: 2.7 weeks).
| NOSE Score . | Improvement . | |||
|---|---|---|---|---|
| Patient . | Before . | After . | Level (%) . | Period (weeks) . |
| 1 | 35 | 0 | 100 | 4 |
| 2 | 90 | 5 | 94.4 | 4 |
| 3 | 65 | 10 | 84.6 | 1 |
| 4 | 80 | 5 | 93.8 | 4 |
| 5 | 90 | 5 | 94.4 | 1 |
| 6 | 90 | 0 | 100 | 2 |
| Average | 75 | 4.2 | 94.5 | 2.7 |
| NOSE Score . | Improvement . | |||
|---|---|---|---|---|
| Patient . | Before . | After . | Level (%) . | Period (weeks) . |
| 1 | 35 | 0 | 100 | 4 |
| 2 | 90 | 5 | 94.4 | 4 |
| 3 | 65 | 10 | 84.6 | 1 |
| 4 | 80 | 5 | 93.8 | 4 |
| 5 | 90 | 5 | 94.4 | 1 |
| 6 | 90 | 0 | 100 | 2 |
| Average | 75 | 4.2 | 94.5 | 2.7 |
The NOSE scale scores for each patient before and after INES are presented, along with the level and period of improvement. The computed average of each of reported parameters is also included.
| NOSE Score . | Improvement . | |||
|---|---|---|---|---|
| Patient . | Before . | After . | Level (%) . | Period (weeks) . |
| 1 | 35 | 0 | 100 | 4 |
| 2 | 90 | 5 | 94.4 | 4 |
| 3 | 65 | 10 | 84.6 | 1 |
| 4 | 80 | 5 | 93.8 | 4 |
| 5 | 90 | 5 | 94.4 | 1 |
| 6 | 90 | 0 | 100 | 2 |
| Average | 75 | 4.2 | 94.5 | 2.7 |
| NOSE Score . | Improvement . | |||
|---|---|---|---|---|
| Patient . | Before . | After . | Level (%) . | Period (weeks) . |
| 1 | 35 | 0 | 100 | 4 |
| 2 | 90 | 5 | 94.4 | 4 |
| 3 | 65 | 10 | 84.6 | 1 |
| 4 | 80 | 5 | 93.8 | 4 |
| 5 | 90 | 5 | 94.4 | 1 |
| 6 | 90 | 0 | 100 | 2 |
| Average | 75 | 4.2 | 94.5 | 2.7 |
The NOSE scale scores for each patient before and after INES are presented, along with the level and period of improvement. The computed average of each of reported parameters is also included.
Symptom-specific analysis
Despite the significant overall improvement, individual NOSE criteria (nasal congestion, obstruction, sleep disturbances, etc.) did not show statistically significant changes (P > 0.05 for all items; Table 2). However, postoperative median scores for all individual criteria dropped to 0 (no symptoms), suggesting clinically meaningful symptom resolution despite limited statistical power.
Patient satisfaction
All patients reported high satisfaction with functional outcomes, correlating with the observed NOSE score reductions.
Surgical technique: The intra nasal endoscopic septoplasty
Our INES technique is specifically indicated for selected unilateral septum deviation. The procedure is particularly suitable for unilateral deviations with associated septal spurs, corresponding to Mladina type 5 and 6 deviations that affect the nasal patency (Fig. 1).
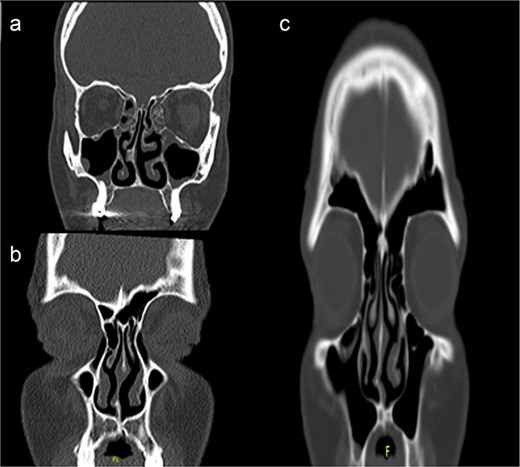
Computed tomography scans showing unilateral nasal obstruction caused by septal spurs, corresponding to Mladina type 5 (lateral nasal wall contact) and type 6 (bilateral spurs) nasal septum deviations.
The procedure begins with proper patient positioning. The patient is placed supine with the head elevated 15°–30° and mild neck extension. The head is stabilized in the midline position to ensure optimal surgical access and visualization throughout the procedure.
Nasal decongestion pack anesthesia is administered using 1% lidocaine with 1:100 000 epinephrine. The solution is carefully infiltrated at the site of deviation and along the planned incision line. Adequate time is allowed for optimal vasoconstriction before proceeding with the surgical steps.
The surgical approach begins with endoscopic visualization of the deviated segment (Fig. 2).
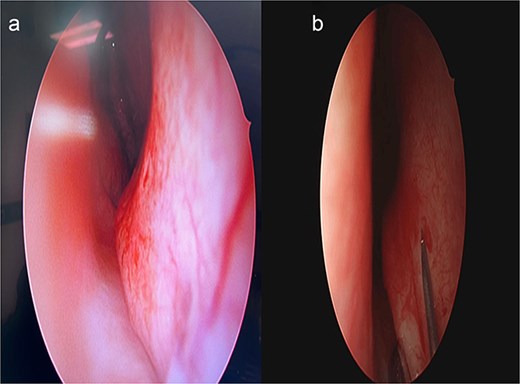
Intraoperative endoscopic view of the deviated nasal septum prior to correction.
Unlike traditional techniques that require extensive septal exposure using kilian or hemitransfixasion incisions, our INES approach utilizes a targeted horizontal incision directly over the deviated from posterior to anterior (Fig. 3). Through this focused incision, superior and inferior mucosal flaps are carefully elevated, limiting the dissection to the deviated area only. This conservative approach maintains the integrity of the contralateral mucoperichondrium and preserves the surrounding normal septal architecture.
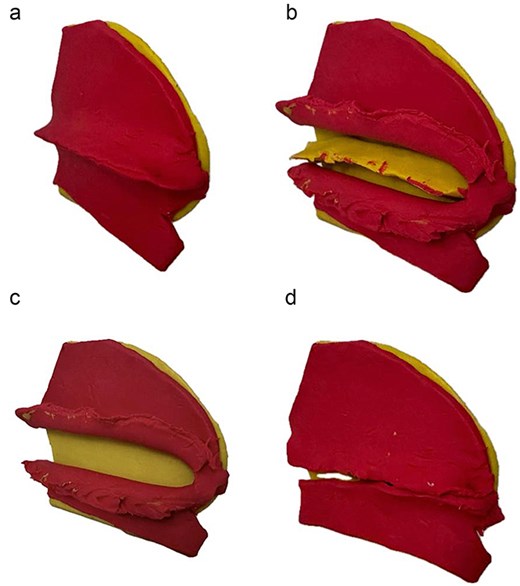
Stepwise illustration of the INES technique. (a) Deviated segment identification; (b) limited mucosal incision and flap elevation; (c) targeted resection of deviated cartilage; (d) mucosal closure without using Silastic sheets/suturing.
Under direct endoscopic visualization, the deviated cartilage and/or bone is precisely identified and resected. This focused correction allows for removal of only the pathological segment while maintaining the structural support of the remaining septum. Meticulous hemostasis is maintained throughout the procedure to ensure optimal visualization and surgical precision (Video 1).
Upon completion of the septal correction, the mucosal flaps are reapproximated. One of the distinctive features of this technique is that routine sialstic sheths are typically not required in most of the patients, although quilting sutures may be placed if deemed necessary based on individual case requirements.
Post-operative care includes saline nasal sprays and head elevation. Patients are typically followed up at 1 week, 1 month, and 6 months postoperatively to assess healing and functional outcomes (Fig. 4).
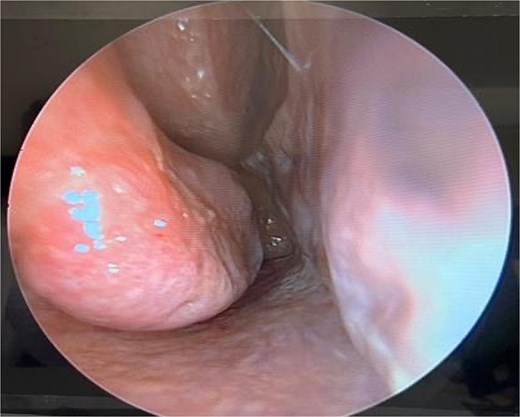
Six-month postoperative follow-up endoscopic view demonstrating healed mucosa and patent nasal airway.
Discussion
Our INES technique represents a modification of the limited septoplasty approach traditionally used in functional endoscopic sinus surgery [5]. While the concept of limited septoplasty is not new, our technique specifically addresses selected unilateral septum deviation which are at the level of the inferior turbinate, an area crucial for nasal airflow dynamics [6, 7].
We classified septal deviations using Mladina’s classification system, which divides DNS into seven different categories [8]. When the deviation impacts the inferior turbinate region, specifically type 5 deviations (unilateral deformity of the basal septal crest) and type 6 deviations (prominent unilateral basal septal crest with contralateral septal deformity) are the target of our approach.
The conventional septoplasty technique typically involves bilateral mucosal flap elevation and extensive cartilage manipulation [9]. In contrast, our approach focuses on targeted correction through a single-sided approach, specifically addressing the deviation at the level of the inferior turbinate region, and resecting only the deviated part of the septum. This selective approach has shown promising results in our series of cases.
Our case series highlights several advantages of this modified technique. Notably, the operative time is significantly reduced, averaging 10–15 min with the INES technique compared to a minimum of 30 min with the conventional approach based on our experience with both techniques. This reduction is attributed to the limited dissection and single-sided access.
Second, all patients showed marked improvement in their NOSE scores, with reductions ranging from 84.6% to 100%, comparable to outcomes reported in conventional septoplasty studies [1, 10]. Notably, the improvement was observed within a short period of time, with patients reporting significant relief in an average of 2.7 weeks. This rapid recovery may be attributed to the absence of a silastic sheath, reduced secretions and edema, the maintenance of a patent airway, and enhanced patient comfort resulting from minimal resection and limited manipulation of the nasal anatomy.
The preservation of septal anatomy with little tissue manipulation is a significant benefit of our approach. While achieving the intended functional benefit, we preserve the septum’s structural integrity by avoiding bilateral mucosal flap elevation and substantial cartilage excision usually done in the traditional endoscopic septoplasty [11]. Additionally, our method typically does not usually require transseptal sutures or silastic sheets, which are frequently utilized in traditional septoplasty [10, 12, 13].
The success of this technique relies heavily on proper patient selection and precise surgical execution. While not suitable for all types of septal deviations, in appropriately selected cases, this modified approach provides excellent outcomes with minimal surgical trauma and reduced post-operative complications.
Approximately 30% of patients who presents with a deviated nasal septum, notably those with localized deviation at the level of the inferior turbinate, are excellent candidates for this treatment, according to our experience.
It is crucial to recognize this technique has a several limits. This method is not suitable for every septal deviation, especially those that involve several regions or have significant caudal dislocation. Patient selection is crucial, and careful preoperative evaluation is necessary to identify suitable candidates for this modified approach.
This case series demonstrates significant overall improvement in nasal obstruction symptoms with INES treatment, thus providing preliminary evidence supporting the efficacy of INES in reducing symptom severity. However, the study is limited by its small sample size, which affects the generalizability of the results. Additionally, no significant differences were observed in individual NOSE scale criteria, indicating potential variability in symptom-specific outcomes. Additionally, the lack of long-term follow-up further limits the ability to assess the sustained effectiveness of the INES technique.
Conclusion
The INES technique offers a minimally invasive, targeted approach for managing selected unilateral septal deviations, particularly Mladina types 5 and 6. By focusing on limited dissection and single-sided correction, this method preserves nasal anatomy, reduces surgical trauma, and shortens recovery time. The INES technique performed on the participants included in this case series exhibited significant overall improvements in nasal obstruction symptoms, with reductions in NOSE scores, and significant decrease in cumulative weighted NOSE scores. However, the small sample size and lack of significant changes in individual NOSE scale criteria highlight the need for further research. Future studies with larger populations and extended follow-up periods are warranted to validate these findings and explore the long-term potential of INES as a promising alternative to traditional septoplasty, offering reduced morbidity and enhanced recovery for appropriately selected patients.
Conflict of interest statement
No conflict of interest.
Funding
No funding was received for this case report.
Consent
Consent was obtained for this study.



