-
PDF
- Split View
-
Views
-
Cite
Cite
Tomás Marín-Cuartas, Steffen Pönitz, Steffi Scholz, Jörg-Peter Ritz, Judith Sporn, Jana Protzel, Hepatic rupture as a life-threatening emergency and rare complication of CPR with the CORPULS device, Journal of Surgical Case Reports, Volume 2025, Issue 6, June 2025, rjaf409, https://doi.org/10.1093/jscr/rjaf409
Close - Share Icon Share
Abstract
Cardiopulmonary resuscitation (CPR) is a life-saving intervention to restore circulation in cardiac arrest patients, with chest compressions being its cornerstone. However, CPR is associated with complications, predominantly chest wall injuries such as rib and sternum fractures. Rarely, intra-abdominal injuries, including liver rupture, can occur, posing life-threatening bleeding risks that require emergent intervention. Recognition of these less common complications can lead to significant improvements in post-CPR protocols and patient outcomes. Raising awareness of visceral injuries after resuscitation highlights the critical need for systematic evaluation and timely intervention. Here, we present a case of a patient with hepatic laceration following CPR with a CORPULS system, successfully identified and managed through a multidisciplinary approach. We propose the adoption of a structured post-CPR abdominal assessment protocol in high-risk patients who have undergone resuscitation.
Introduction
Cardiopulmonary resuscitation (CPR) is a life-saving procedure to restore vital functions in patients with cardiac and respiratory arrest. Chest compressions are a critical component of CPR, but can cause complications, particularly skeletal injuries like rib and sternum fractures [1–3]. Automated devices like CORPULS, introduced in 2015, improve compression consistency and efficiency over manual CPR [4]. The CORPULS system includes a backplate under the patient and a piston-based compression module above the chest, delivering guideline-consistent compressions with proper depth and rate. Though rare, intra-abdominal injuries, including liver rupture, can be life-threatening [1, 5], causing significant bleeding and requiring emergent surgery. Early recognition and management are vital to improving patient outcomes following successful resuscitation.
Case presentation
A 66-year-old female patient with a medical history of X-linked adrenomyelopathy and multiple cervical and thoracic disc herniations, primarily wheelchair-bound, presented with dyspnea and chest pain while sitting on the toilet. Paramedics noted tachycardia, cold sweats, nausea, and neck pressure. An ECG revealed nonspecific ST-segment elevations. During transport, the patient developed ventricular fibrillation, prompting immediate resuscitation. Suspecting acute coronary syndrome, intravenous acetylsalicylic acid and 5000 IU of heparin were administered. The patient arrived at the emergency department ~15–20 minutes after resuscitation began.
Upon arrival, resuscitation continued using the CORPULS CPR system. The patient was admitted through the shock room of the chest pain unit. Echocardiography suggested an acute posterior myocardial infarction. According to our company’s extracorporeal cardiopulmonary resuscitation (eCPR) protocol, we evaluated possible exclusion criteria for ECLS therapy.
Due to the absence of return of spontaneous circulation (ROSC), an interdisciplinary decision according to our e-CPR protocol was made to implement veno-arterial extracorporeal membrane oxygenation (VA-ECMO). During ongoing mechanical resuscitation, the patient was transferred to the catheterization laboratory, where coronary angiography identified moderate to severe stenosis of the right coronary artery. Two drug-eluting stents were successfully deployed.
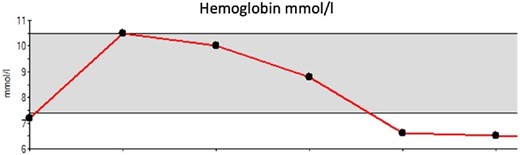
Subsequently, due to a noticeable drop in hemoglobin (Fig. 1) and significant abdominal distention prompted an eFAST ultrasound, which revealed free fluid around the liver. A contrast-enhanced computed tomography (CT) scan of the thorax and abdomen demonstrated a central and peripheral pulmonary artery embolism with a massive thrombus burden, as well as extensive free fluid in all abdominal quadrants. Fresh blood adjacent to the ventral margin of the left liver lobe indicated parenchymal damage and capsular injury (Fig. 2). An emergency laparotomy confirmed a laceration of the left liver lobe, which was repaired using Vicryl 0 sutures and TachoSil. Postoperatively, an interventional thrombectomy of the pulmonary circulation was performed.

CT of the abdomen. Significant amounts of free fluid in all quadrants (arrows), with fresh blood adjacent to the ventral edge of the left liver lobe (star).
The patient recovered satisfactorily with a good neurological outcome, was tracheotomized due to critical illness polyneuropathy, and was discharged to a rehabilitation center seven days later.
Discussion
Chest compressions are a fundamental component of CPR and play a crucial role in survival following cardiac arrest. However, they are a traumatic procedure frequently associated with complications of varying severity, and any complication more serious than soft tissue trauma is undesirable [1]. The most reported CPR-related injuries are rib and sternal fractures, which do not usually contribute to patient mortality [4–6]. The reported incidence of rib and sternum fractures varies significantly in the literature, ranging from 28% to 85% and 30% to 71%, respectively [4, 6–8]. In contrast, intra-abdominal injuries are rare but can have severe consequences, including liver and spleen laceration, gastric dilatation, and gastric perforation [1, 9]. Liver injury is the most frequent intra-abdominal complication related to CPR, with a reported incidence of approximately 0.6% [1, 5, 10]. A single-center observational study found major liver injury in 15 of 2558 cardiac arrest patients (0.6%), with 40% of these cases only identified post-mortem [2].
Risk factors for CPR-related liver injury may include improper hand positioning, heart and liver failure leading to hepatomegaly, and anticoagulation therapy. However, due to the liver's size and location, even correctly performed chest compressions can potentially cause injury. While any part of the liver can be affected, damage to the left lobe appears to be more common, likely due to its close anatomical relationship with the lower sternum [1, 4, 9, 11].
Early recognition of CPR-related hepatic injuries is challenging, as most resuscitated patients have a reduced level of consciousness and cannot communicate symptoms. Furthermore, intra-abdominal bleeding may progress slowly, with hypovolemic signs emerging minutes to hours after CPR, often mimicking the hemodynamic instability associated with post-cardiac arrest syndrome [2, 5, 7]. This diagnostic challenge increases the risk of delayed intervention, which can be fatal.
Automated CPR devices, such as the CORPULS CPR or LUCAS device, offer advantages in maintaining high-quality compressions, however, their potential to cause iatrogenic trauma must not be overlooked [8, 12]. Iatrogenic trauma should be considered a differential diagnosis in cases of unexpected cardiovascular collapse in resuscitated patients, particularly those receiving thrombolytic therapy, as even minor intra-abdominal injuries can result in massive hemorrhage [7, 9, 10].
Post-mortem investigations by other authors have revealed that major visceral injuries often go undetected, with none of these studies reporting clinical suspicion during life [10].
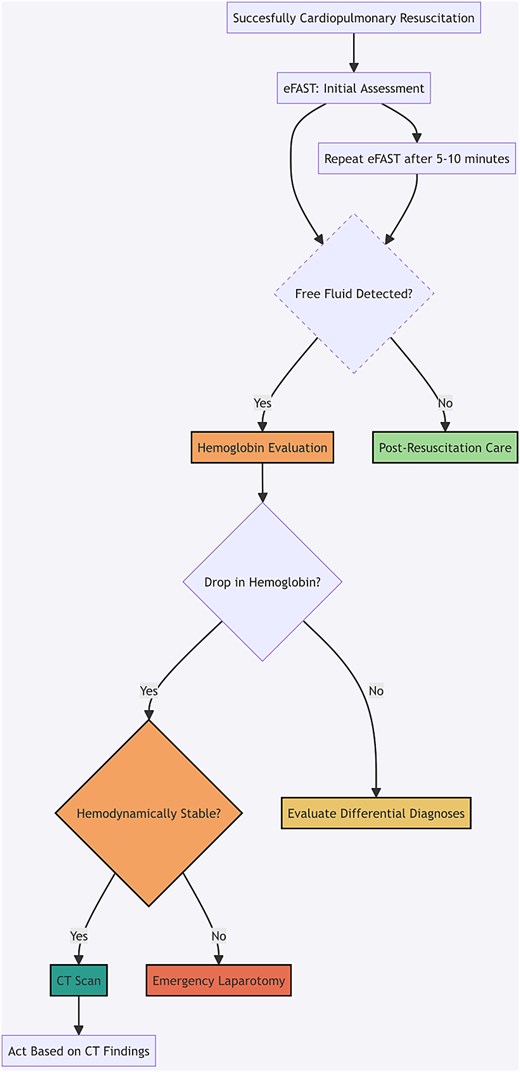
A quantifiable measurement like hematocrit can serve as a useful indicator in clinical assessment. Hematocrit levels are easily monitored through regular blood tests, and a significant drop should prompt further diagnostic investigation [9]. In cases of suspected internal bleeding or organ injury, such as after prolonged CPR, particularly in high-risk patients or in patients receiving thrombolytic, anticoagulant, or antiplatelet therapy, clinical suspicion should be heightened. Bedside abdominal sonography can quickly detect free intraabdominal fluid. If findings are inconclusive or if clinical suspicion remains high, repeat examinations or advanced imaging, such as CT, should be considered to ensure a timely intervention [2, 10] (Fig. 3).
Conclusion
CPR-related visceral injuries, though rare, can have life-threatening consequences, particularly when undetected. Due to the liver’s anatomical vulnerability and predisposing factors such as hepatomegaly or anticoagulation therapy, even correctly performed chest compressions can cause significant damage. The challenge of early diagnosis, compounded by altered consciousness in resuscitated patients, increases the risk of delayed intervention and fatal outcomes. While automated CPR devices improve compression quality, they also carry a risk of visceral trauma. To mitigate these risks, heightened clinical suspicion, routine hemoglobin monitoring, and early imaging, such as eFAST or CT in high-risk patients, should be integrated into post-CPR evaluation protocols. Rapid recognition and management of these complications through a multidisciplinary approach are essential to improve post-resuscitation outcomes.
Conflict of interest statement
None declared.
Funding
None declared.
Declaration of generative AI and AI-assisted technologies in the writing process
During the preparation of this work, the author(s) used ChatGPT in order to correct grammar and language. After using this tool, the author(s) reviewed and edited the content as needed and take(s) full responsibility for the content of the publication.



