-
PDF
- Split View
-
Views
-
Cite
Cite
Ali Toffaha, Hafiz Bilal Zafar, Hamza A Abdul-Hafez, Mahmood Al-Dhaheri, Mohamed Abunada, Amjad Parvaiz, An unusual case of isolated brain metastasis with impending brain herniation from sigmoid colon cancer: case report and review of literature, Journal of Surgical Case Reports, Volume 2025, Issue 6, June 2025, rjaf394, https://doi.org/10.1093/jscr/rjaf394
Close - Share Icon Share
Abstract
Colorectal carcinoma with a finding of isolated brain metastasis is rare. Furthermore, neurologic symptoms secondary to oligometastasis to the brain are very rare initial presentations for colorectal cancer. Hence, it is uncommon to do brain imaging in the initial staging of colon carcinoma. We present an unusual case of a patient who initially presented with a headache. Laboratory tests revealed mild anemia. Brain imaging revealed a mass in the parietal lobe; hence, neurosurgery was performed with resection of the mass. Histopathology showed it’s colonic in origin. Colonoscopy revealed adenocarcinoma in the sigmoid colon and a staging computed tomography scan showed no distant metastases. This case report highlights the unusual presentation of an isolated brain metastasis secondary to primary colon carcinoma. Any patient with a primary colon tumor who complains of neurologic symptoms should be considered for brain evaluation to minimize the risk of overlooking such important finding.
Introduction
Colorectal carcinoma (CRC) is the third most common cancer and the second leading cause of cancer-related death in the United States [1]. CRC usually presents with gastrointestinal (GI) symptoms that include bleeding per rectum, abdominal pain, and changes in bowel habits, with many patients being anemic [2]. Approximately up to 22% of patients with CRC have metastatic disease at the time of initial presentation [1]. The most common site of single-site metastasis at the time of diagnosis is the liver (60%) and the least common is the brain (1%) [3]. Brain metastases (BMs), regardless of the primary tumor, usually present with headache [4]. However, isolated BM of CRC without liver or lung involvement is very rare [3].
We report a unique case who presented with headache and vomiting due to an isolated BM secondary to sigmoid carcinoma.
Case report
A 47-year-old woman presented to the emergency department complained of severe headache for 1 month. The headache had been worsening over the last 3 days, prompted patient to sought medical advice. The headache was associated with vomiting but there were no other neurological symptoms. Past medical history revealed of asymptomatic atrial septal defect, following with cardiologist, and iron deficiency anemia, receiving iron supplements. She also underwent bariatric weight loss surgery 4 years ago. Her social, environmental, family, and employment history were unremarkable. She never smoked or consumed alcohol.
At baseline, her vital signs were within normal range, physical examination was unremarkable, and there were no focal neurologic deficits. Laboratory tests, including the complete metabolic panel, were within normal range except for the low hemoglobin (10.2 g/dl). Due to the severity and chronicity of her symptoms, a brain computed tomography (CT) scan was performed which showed a lesion of the right parietal lobe, surrounding edema, and central hyperdense area, with midline shift and effacement of the ipsilateral right lateral ventricle. Magnetic resonance imaging (MRI) of the brain showed an intra-axial lesion, measuring of 2.6 × 2.3 × 2.6 cm, in the right parietal lobe with small frontal extent. Additionally, it was surrounded by significant vasogenic edema, showed mass effect evidenced by effacement of adjacent sulci, compression of right lateral ventricle, 6 mm leftward shift of midline structures, and mild herniation of right cranial vault (Fig. 1). The working diagnosis was a brain tumor with mass effect, so the patient underwent right parietal craniotomy and resection of the intra-axial solid tumor. Intraoperative frozen section showed adenocarcinoma with clear resection margins. The postoperative course was uneventful, and she was discharged home after 7 days. Surprisingly, final histopathological report showed metastatic adenocarcinoma with morphological and immunohistochemical features favoring a colorectal origin.
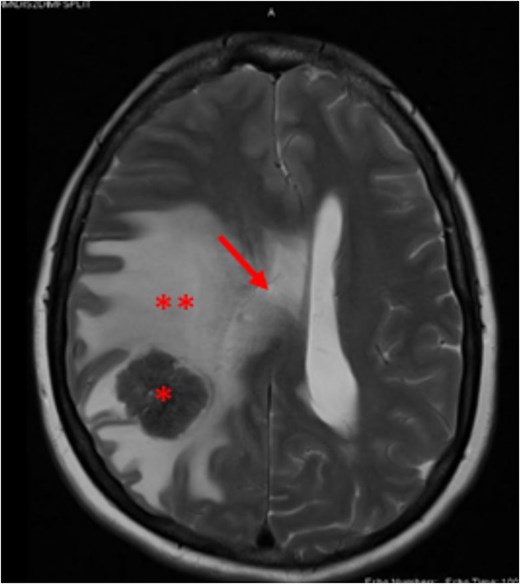
Brain MRI T2 weighted image, showing right parietal lobe lesion (asterisk), surrounded by edema (**) and causing right lateral ventricular compression with midline shift (arrow).
The case was discussed in the neuro-oncology multidisciplinary team (MDT) meeting, which recommended colonoscopy and stereotactic radiosurgery (SRS) of the tumor bed. SRS was performed with 20 Gray (Gy) in a fraction. Upper and lower endoscopies were performed which showed a sigmoid tumor (Fig. 2), endoscopic biopsy confirmed a moderately differentiated adenocarcinoma. Staging CT scans of the chest and abdomen along with positron emission tomography (PET) CT showed no metastasis (Fig. 3). Baseline tumor markers, including carcinoembryonic antigen (CEA) and cancer antigen (CA19-9), were within normal range. She was reviewed at the colorectal MDT and planned for neoadjuvant chemotherapy (leucovorin, Fluorouracil, and Oxaliplatin (FOLFOX) 4 cycles), followed by surgical resection of the primary sigmoid tumor. The patient completed her chemotherapy cycles and follow-up brain imaging revealed no new brain lesions. She subsequently underwent sigmoid colectomy with uneventful recovery.

Circumferential, non-obstructing, irregular growth in the sigmoid colon around 35 cm from the anal verge.
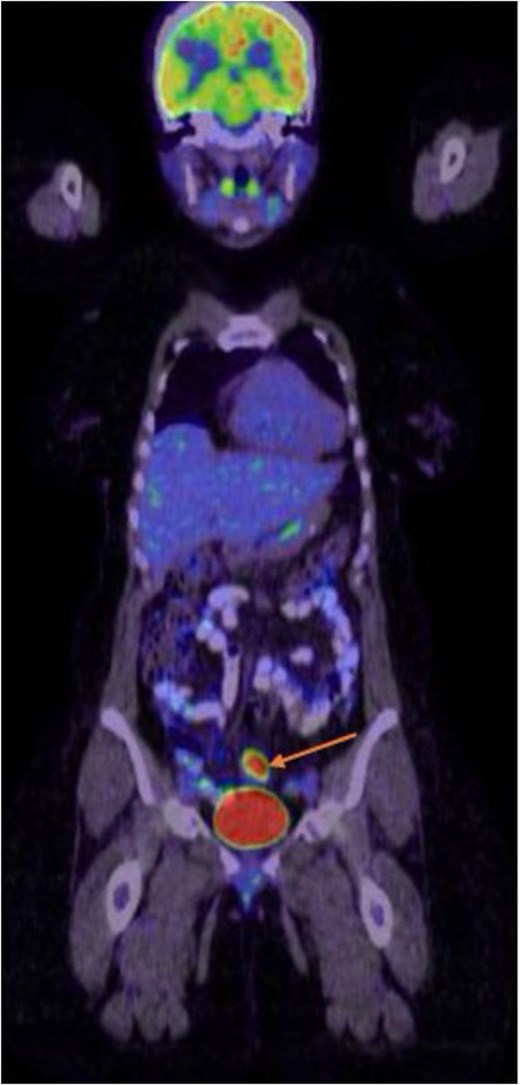
Whole body PET CT scan showing sigmoid colonic tumor with intense metabolic activity. No detectable locoregional lymph nodal or distant metastasis.
Discussion
Metastatic brain disease presents with a range of symptoms from ataxia, headache, dizziness, seizures, dysphagia to mental status changes [5]. In most published reports of isolated BM due to CRC, patients presented with a symptomatic brain mass and underwent craniotomy and resection, with histopathology showing metastasis from a primary GI source that was later found to be colorectal in origin. The clinical presentation of our case followed similar patterns as previously reported (Table 1).
Literature review for colorectal cancer cases presented initially with isolated brain metastasis
| Studya . | Sex . | Age . | PH . | Presentation . | D . | Hb . | Brain imaging . | Colonoscopy . | Surgery . | Radiation . | Histo . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Current study Qatar 2020 | F | 47 y | Anemia ASD | Headache, vomiting | 1 m | 10.2 | R parietal | Sigmoid | Craniotomy | SRS | Adeno T3N2M1 |
| Esplin and Hubbard [6] USA 2016 | F | 55 y | UR | Hand incoordination, gait instability | 2 w | 11 | Cerebellum | Right colon | Craniotomy R hemicolectomy | WBRT | Adeno |
| Gómez Raposo [12] Spain 2007 | M | 81 y | DM, COPD | Dysarthria | NR | NR | R parietal L front-parietal | NR | Emergency laparotomy resection of cecal adenocarcinoma | NR | Adeno T4N2M1 |
| Ruiz-Tovar [13] Spain 2010 | M | 55 y | Familial colonic polyposis | Rotation of eyes and head to left, LOC, GTCS | 1 d | NR | R frontal | Right colon | Craniotomy excision R hemicolectomy | NR | Adeno T3N0M1 |
| Erhamamcı [14] Turkey 2015 | M | 52 y | DM | L hemiparesis | NR | NR | R parietal | PET scan found the primary | Craniectomy excision biopsy Subtotal colectomy | WBRT | Adeno T3N1M1 |
| Goto [15] Japan 2014 | F | 75 | NK | L hemiparesis | NR | NK | R frontal | Left colon | Craniotomy Hemicolectomy Re-resection of BM | WBRT | Adeno |
| Studya . | Sex . | Age . | PH . | Presentation . | D . | Hb . | Brain imaging . | Colonoscopy . | Surgery . | Radiation . | Histo . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Current study Qatar 2020 | F | 47 y | Anemia ASD | Headache, vomiting | 1 m | 10.2 | R parietal | Sigmoid | Craniotomy | SRS | Adeno T3N2M1 |
| Esplin and Hubbard [6] USA 2016 | F | 55 y | UR | Hand incoordination, gait instability | 2 w | 11 | Cerebellum | Right colon | Craniotomy R hemicolectomy | WBRT | Adeno |
| Gómez Raposo [12] Spain 2007 | M | 81 y | DM, COPD | Dysarthria | NR | NR | R parietal L front-parietal | NR | Emergency laparotomy resection of cecal adenocarcinoma | NR | Adeno T4N2M1 |
| Ruiz-Tovar [13] Spain 2010 | M | 55 y | Familial colonic polyposis | Rotation of eyes and head to left, LOC, GTCS | 1 d | NR | R frontal | Right colon | Craniotomy excision R hemicolectomy | NR | Adeno T3N0M1 |
| Erhamamcı [14] Turkey 2015 | M | 52 y | DM | L hemiparesis | NR | NR | R parietal | PET scan found the primary | Craniectomy excision biopsy Subtotal colectomy | WBRT | Adeno T3N1M1 |
| Goto [15] Japan 2014 | F | 75 | NK | L hemiparesis | NR | NK | R frontal | Left colon | Craniotomy Hemicolectomy Re-resection of BM | WBRT | Adeno |
aFor space considerations, only the first author is cited; Adeno: adenocarcinoma; ASD: atrial septal defect; COPD: chronic obstructive pulmonary disease; D: duration of symptoms; d: days; h: hour/s; DM: diabetes mellitus; GTCS: generalized tonic clonic seizure; Hb: hemoglobin in mg/dl; Histo: histology; L: left; M: male; LOC: loss of consciousness; m: month/s; NK: not known; NR: not reported; PH: physical examination; R: right; SRS: stereotactic surgery; UR: unremarkable; w: week/s; WBRT: whole brain radiotherapy; y: year/s.
Literature review for colorectal cancer cases presented initially with isolated brain metastasis
| Studya . | Sex . | Age . | PH . | Presentation . | D . | Hb . | Brain imaging . | Colonoscopy . | Surgery . | Radiation . | Histo . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Current study Qatar 2020 | F | 47 y | Anemia ASD | Headache, vomiting | 1 m | 10.2 | R parietal | Sigmoid | Craniotomy | SRS | Adeno T3N2M1 |
| Esplin and Hubbard [6] USA 2016 | F | 55 y | UR | Hand incoordination, gait instability | 2 w | 11 | Cerebellum | Right colon | Craniotomy R hemicolectomy | WBRT | Adeno |
| Gómez Raposo [12] Spain 2007 | M | 81 y | DM, COPD | Dysarthria | NR | NR | R parietal L front-parietal | NR | Emergency laparotomy resection of cecal adenocarcinoma | NR | Adeno T4N2M1 |
| Ruiz-Tovar [13] Spain 2010 | M | 55 y | Familial colonic polyposis | Rotation of eyes and head to left, LOC, GTCS | 1 d | NR | R frontal | Right colon | Craniotomy excision R hemicolectomy | NR | Adeno T3N0M1 |
| Erhamamcı [14] Turkey 2015 | M | 52 y | DM | L hemiparesis | NR | NR | R parietal | PET scan found the primary | Craniectomy excision biopsy Subtotal colectomy | WBRT | Adeno T3N1M1 |
| Goto [15] Japan 2014 | F | 75 | NK | L hemiparesis | NR | NK | R frontal | Left colon | Craniotomy Hemicolectomy Re-resection of BM | WBRT | Adeno |
| Studya . | Sex . | Age . | PH . | Presentation . | D . | Hb . | Brain imaging . | Colonoscopy . | Surgery . | Radiation . | Histo . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Current study Qatar 2020 | F | 47 y | Anemia ASD | Headache, vomiting | 1 m | 10.2 | R parietal | Sigmoid | Craniotomy | SRS | Adeno T3N2M1 |
| Esplin and Hubbard [6] USA 2016 | F | 55 y | UR | Hand incoordination, gait instability | 2 w | 11 | Cerebellum | Right colon | Craniotomy R hemicolectomy | WBRT | Adeno |
| Gómez Raposo [12] Spain 2007 | M | 81 y | DM, COPD | Dysarthria | NR | NR | R parietal L front-parietal | NR | Emergency laparotomy resection of cecal adenocarcinoma | NR | Adeno T4N2M1 |
| Ruiz-Tovar [13] Spain 2010 | M | 55 y | Familial colonic polyposis | Rotation of eyes and head to left, LOC, GTCS | 1 d | NR | R frontal | Right colon | Craniotomy excision R hemicolectomy | NR | Adeno T3N0M1 |
| Erhamamcı [14] Turkey 2015 | M | 52 y | DM | L hemiparesis | NR | NR | R parietal | PET scan found the primary | Craniectomy excision biopsy Subtotal colectomy | WBRT | Adeno T3N1M1 |
| Goto [15] Japan 2014 | F | 75 | NK | L hemiparesis | NR | NK | R frontal | Left colon | Craniotomy Hemicolectomy Re-resection of BM | WBRT | Adeno |
aFor space considerations, only the first author is cited; Adeno: adenocarcinoma; ASD: atrial septal defect; COPD: chronic obstructive pulmonary disease; D: duration of symptoms; d: days; h: hour/s; DM: diabetes mellitus; GTCS: generalized tonic clonic seizure; Hb: hemoglobin in mg/dl; Histo: histology; L: left; M: male; LOC: loss of consciousness; m: month/s; NK: not known; NR: not reported; PH: physical examination; R: right; SRS: stereotactic surgery; UR: unremarkable; w: week/s; WBRT: whole brain radiotherapy; y: year/s.
Although most of the reported patients had focal neurological deficits at initial presentation (Table 1), the neurological examination in our patient was normal. Our case had iron deficiency anemia, which had been treated with iron supplements for several years. Since she had undergone bariatric surgery for weight loss, this anemia could be due to the long-term complication of the surgery itself. Brandt reported a case that had a hemoglobin level of 11 mg/dl [6]. However, most of the published data we came across did not report the hemoglobin levels of their patients (Table 1).
The imaging findings of our patient showed a lesion of the right parietal lobe with mass effect, the parietal lobe was the most common involved location in the previous reports, followed by cerebellum and frontal lobe (Table 1).
The median time of detection of BM after the diagnosis of CRC is 22 to 36 months [7], it is very uncommon to find isolated BM as a presenting complaint, as in our case, therefore the protocols for the treatment of BM due to CRC are less defined in the literature [8].
Treatment options for BM from CRC include resection, SRS, whole brain radiation (WBRT), systemic chemotherapy, and palliative care [8].
Suzuki et al. reported 46 patients with curative neurosurgical resection followed by WBRT for BM from CRC. The median overall survival (OS) was 15.2 months and 1-year survival rate was 57% [9]. They listed extracranial metastasis (P = .03), number of brain lesions (P = .001), and no occurrence of secondary brain lesions (P = .02) as significant prognostic factors [9]. Our case had only one brain metastatic focus without extracranial metastases and underwent surgical resection followed by SRS. Similarly, Byrne et al. reported six cases with curative neurosurgery showing the best results with a median survival of 13.2 months, these patients also received adjuvant WBRT or SRS [10].
Koo et al. reported 106 patients who underwent WBRT for BM from CRC. Surgical resection was performed in six patients, and two patients underwent SRS. One patient received systemic therapy, regorafenib before WBRT, while 26 patients received systemic therapy after WBRT. Eleven patients received 5-fluorouracil (5-FU) and oxaliplatin-based treatment, and three different regimens were used in each of the five patient groups: 5-FU and irinotecan-based, capecitabine-based, and other regimens. The median OS was 3.9 months. The 1-year survival rate was 18.2% [11]. Our patient received four cycles of FOLFOX therapy.
For prognosis, older age 65 years, multiple BM, CEA 5 ng/ml, and extracranial metastasis were poor prognostic factors for OS [11]. Our patient is young, had a normal CEA level, and no extracranial metastasis, which puts her in a favorable prognosis. Her recent follow-up showed no new brain lesion.
Conclusions
CRC may present in an atypical presentation that may include neurological abnormalities due to BM. Although it remains a rare initial presentation, CRC may present with neurological symptoms as a single site metastasis. Patients presenting with a brain mass and anemia might have primary colorectal tumor as the source of these findings, warranting GI work up. As more cases of oligometastases to the brain due to colorectal cancer are reported, brain imaging may be required as an initial screening tool to complete staging and avoid overlooking this rare but important finding.
Author contributions
All authors contributed to original drafting, literature search, and data conception. All authors read and approved the final manuscript.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
The authors received no funding from an external source.
Consent
Written informed consent was obtained from the patient for publication and any accompanying images.
References
Forsyth PA, Posner JB. Headaches in patients with brain tumors: a study of 111 patients. Neurology 1993;
- anemia
- computed tomography
- brain herniation
- metastatic malignant neoplasm to brain
- colonoscopy
- colorectal cancer
- adenocarcinoma
- headache
- colonic neoplasms
- laboratory techniques and procedures
- neurologic manifestations
- sigmoid colon
- brain
- colon
- neurosurgical procedures
- parietal lobe
- colon cancer
- brain imaging
- metastasis, distant
- large intestine adenocarcinoma
- histopathology tests
- sigmoid cancer
- oligometastasis



