-
PDF
- Split View
-
Views
-
Cite
Cite
Zahraa Almuhanna, Zinab Bohulaigah, Hussain Alkhawaja, Hadeel Aljafar, Posterior trachea wall erosion: a case report and literature review of a catastrophic complication of cuff overinflation, Journal of Surgical Case Reports, Volume 2025, Issue 6, June 2025, rjaf361, https://doi.org/10.1093/jscr/rjaf361
Close - Share Icon Share
Abstract
Tracheostomy complications range from early to late complications. One of the late complications can be seen with cuff over-inflation that exceeds tracheal capillary perfusion pressure, which leads to segmental tracheomalacia and rarely, tracheal wall erosion. A 40-year-old male with amyotrophic lateral sclerosis and mechanical ventilation dependence was found to have a persistent ventilatory leak. Endoscopic examination revealed a large posterior tracheal wall erosion that was confirmed by computed tomography. Conservative management by the placement of a long endotracheal tube through the tracheostoma was chosen. Cuff pressure over 20–25 cm H₂O, which exceeds tracheal capillary perfusion pressure, increases the risk of tracheal mucosal ischemia. Preventive strategies such as the use of pressure-limiting devices and careful tube selection, should be implemented. Regular implementation of preventive measures along with early identification are essential for avoiding tracheostomy tube complications. This case demonstrates the importance of strict cuff pressure maintenance to avoid tracheal wall injuries.
Introduction
Tracheostomy is essential for patients who need prolonged mechanical ventilation or those with upper airway obstruction. Despite its life-saving benefits, it can lead to severe complications. Cuff over-inflation can cause pressure necrosis of the tracheal mucosa, leading to tracheal wall erosion and tracheomalacia [1].
Maintaining appropriate cuff pressure is vital to prevent tracheal injuries. Studies have shown that continuous monitoring and control of endotracheal cuff pressure can significantly reduce the risk of tracheal ischemia [2]. In an experimental study involving mechanically ventilated piglets, those with continuous cuff pressure control exhibited fewer tracheal lesions compared to those with manual control, showing the importance of continuous monitoring in clinical practice [3].
Another case report described a patient who developed tracheal wall necrosis and subsequent stenosis due to cuff over-inflation, necessitating the insertion of an endotracheal prosthesis. This case illustrated the preventable nature of such complications through vigilant cuff pressure management [1].
Tracheoesophageal fistula (TEF) and tracheo-innominate artery fistula (TIF) are rare, but often fatal complications of tracheostomy. Over-inflation of the tracheostomy tube cuff can contribute to their development by causing pressure necrosis of the tracheal wall [4]. Patient-specific factors, such as pre-existing tracheal wall weakness, can exacerbate the risk of tracheal rupture associated with cuff overinflation. A case report detailed a patient who suffered tracheal rupture related to endotracheal intubation after thyroid surgery, massive over-inflation of the cuff was identified as the most likely cause [5]. The current literature on tracheostomy complications lacks detailed case-based insights into rare but severe outcomes like posterior tracheal wall erosion. The current case report provides a comprehensive clinical account of this life-threatening complication, helping to address the gap in understanding its pathophysiology, risk factors, and management strategies.
Case presentations
A 40-year-old male who is known to have amyotrophic lateral sclerosis was admitted to the intensive care unit for ventilatory support. He underwent surgical tracheostomy for long-term mechanical ventilation dependence, a double-lumen tracheostomy tube with an internal diameter of 8 mm and a maximum cuff pressure of 25.4 mm was inserted, post-operative chest X-ray confirmed tube placement (Fig. 1). Six months later, the otolaryngologist on-call was consulted regarding ventilation leak that was evident in the ventilator. Flexible endoscopy through the stoma revealed a significantly dilated trachea with a posterior groove. The tube was changed to size 7 with an extended distal length of 49 mm to bypass the dilated segment. A temporary improvement was noted; however, the leak was noted again, with an inspiratory tidal volume of 800, and an expiratory volume of 135, the cuff pressure was gradually elevated to overcome the leak reaching a maximum of 40 mmHg, with the cuff seen over-inflated in routine supine chest X-ray (Fig. 2). Multiple tube obstruction events happened later, which required rigid bronchoscopy examination under general anesthesia to assess and relieve the obstruction. Intraoperative examination revealed that the obstruction was caused by a large dry blood clot, withdrawal of the tube to examine the trachea further revealed a large posterior tracheal wall defect with exposed thoracic vertebrae. The patient underwent a subsequent contrast-enhanced computed tomography scan (CECT) of the neck and chest which confirmed the intraoperative findings (Fig. 3). The leak was not improving by increasing cuff pressure, consequently, the decision was made to use an armored endotracheal tube size 8 at a lip level of 13 to bypass the defect. This has slightly improved the oxygenation and ventilation of the patient, but it did not eliminate the leak. The general poor health of the patient along with his do-not-resuscitate (DNR) status has led to deterring the decision of surgical tracheal wall repair. The patient was further diagnosed with sepsis due to multiple infection sources including his long-term suprapubic urinary catheter, he eventually had a cardiopulmonary collapse a few weeks later and passed away.

Post-operative frontal portable chest radiograph showing a tracheostomy tube in position above the carina.

Frontal portable chest radiograph showing a tracheostomy tube in satisfactory position above the carina, however, there is a rounded radiolucency at the expected position of the tracheostomy cuff suggestive of tracheostomy tube cuff overinflation. Additionally, there is a small right pleural effusion with adjacent atelectatic changes/ consolidation.
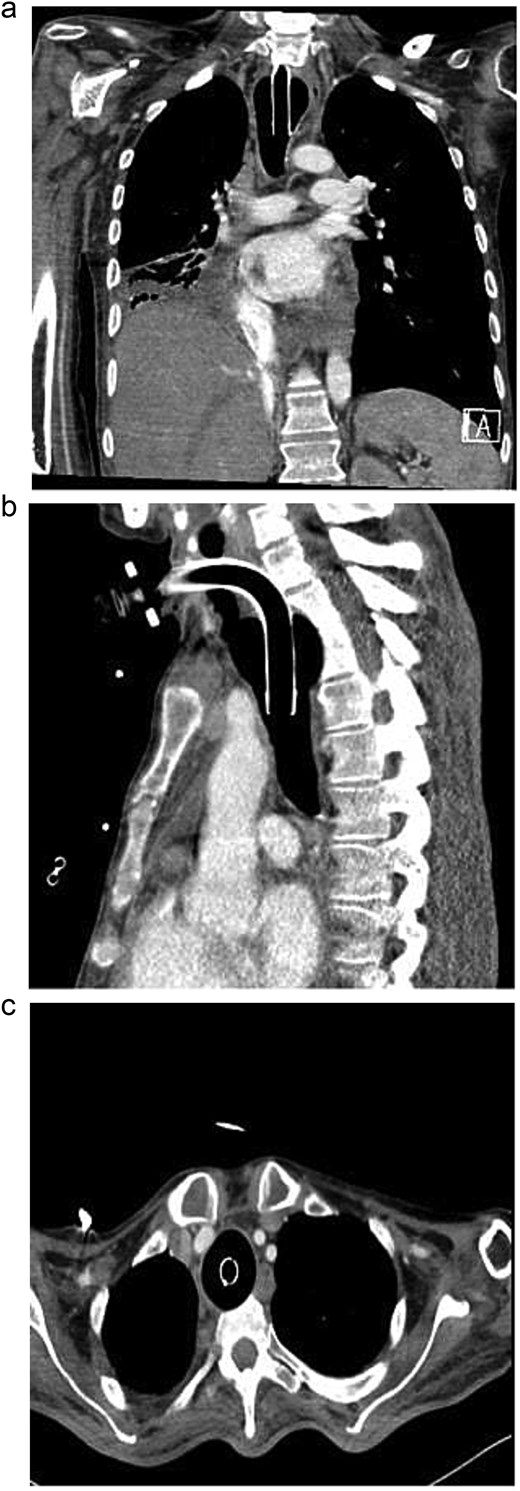
Axial contrast-enhanced chest CT with reformatted coronal and sagittal images showing fusiform dilation of the trachea with scalloping of the anterior surface of thoracic vertebral bodies. Moreover, no appreciable separating soft tissue layer between the tracheostomy cuff and the anterior surface of vertebral bodies.
Discussion
Tracheostomy is a widely performed procedure to secure long-term airway access, but it carries the risk of complications, particularly when cuff overinflation occurs. In this presented case, posterior tracheal wall erosion was observed as a catastrophic complication of excessive cuff pressure, leading to a life-threatening condition. This finding aligns with previously published research indicating that tracheal wall damage is one of the most common adverse outcomes associated with high cuff pressures. Studies have documented similar cases where prolonged and excessive cuff inflation caused tracheal ischemia and necrosis, leading to erosion and fistula formation [6, 7].
Research emphasizes that cuff pressures over 20–25 cm H₂O, which exceeds tracheal capillary perfusion pressure, increase the risk of tracheal mucosal ischemia. Experimental studies have shown that automatic cuff pressure control reduces tracheal lesions compared to manual adjustments, this also demonstrates the importance of using advanced monitoring techniques in clinical practice [8, 9].
Posterior tracheal wall erosion can lead to life-threatening scenarios such as mediastinitis and sepsis. Routine surveillance with imaging or bronchoscopy in patients with prolonged intubation or tracheostomy to detect early signs of tracheal injury could prevent severe outcomes [10].
The patient’s overall condition added complexity to the management of tracheal injury. Literature suggests that patients with neuromuscular disorders are at higher risk of complications due to prolonged intubation and reduced tissue resilience [11].
The management of iatrogenic tracheal wall injury can be divided into conservative and surgical measures. However, no consensus or approved guidelines are present, and an individualized, case-by-case decision can be applied. Surgery is generally indicated in cases where transmural tracheal wall injury, and/or mediastinal or esophageal involvement is evident. Most cases can be managed conservatively regardless of the length and/or location of the injury. Conservative measures include distal placement of the tube to bypass the injury, antibiotics coverage, pressure-controlled low tidal volume ventilation in mechanically ventilated patients, prone positioning, and regular flexible bronchoscopic examination to assess resolution. Tracheal stents can also be applied when possible [12, 13]. Surgical approaches depend on the anatomical location and the extent of the injury. Involvement of the bronchial tree usually requires thoracotomy. Isolated posterior tracheal wall rupture can be managed by either a left cervical approach, or a trans-tracheal approach that can be chosen if a tracheostomy opening already exists. Direct repair of the tracheal wall injury is usually sufficient, and the use of the most external part of the anterior wall of the esophagus as a re-enforcement can be helpful [14].
The inability to surgically repair the tracheal defect due to the patient’s poor health and do-not-resuscitate status further illustrates the importance of preventive measures. Surgical interventions for tracheal injuries, while effective, are often contraindicated in patients with significant comorbidities or poor prognosis. Multiple preventive strategies can be implemented such as the use of pressure-limiting devices, careful tube selection, and staff training to avoid complications from the outset. Published guidelines for tracheostomy care emphasize team-based approaches, regular staff training, and patient-specific care protocols to reduce complications and improve outcomes [15].
Conclusion
A rare complication of posterior tracheal wall erosion due to cuff over-inflation is presented here. Endoscopic examination and complementary imaging were crucial to reach the diagnosis. Regular implementation of preventive measures, including respiratory therapist personnel training, along with early identification and multidisciplinary team approach are essential for avoiding tracheostomy tube complications.
Strengths and limitations
Our study presents a rare but severe complication of posterior tracheal wall erosion caused by tracheostomy tube cuff over-inflation, emphasizing the importance of vigilant cuff pressure monitoring. One of its key strengths lies in the detailed clinical observations and comprehensive evaluation, including imaging and endoscopic findings, which contribute to understanding the pathophysiological mechanisms of tracheal injury. However, the study is limited by its single-case design, which restricts the generalizability of the findings. The absence of a surgical intervention or repair due to the patient’s poor health limits the exploration of therapeutic options. The lack of long-term follow-up data further constrains the assessment of outcomes related to different management strategies.
Future research and directions
Future research should focus on large-scale, multicenter studies to assess the incidence, risk factors, and preventive strategies for tracheal injuries associated with tracheostomy. Investigating the efficacy of automated cuff pressure monitoring systems compared to manual adjustments in preventing complications would provide valuable data to refine clinical guidelines. Exploring minimally invasive interventions for early-stage tracheal injuries and their outcomes could enhance treatment options. Studies focusing on patient-specific factors, such as comorbidities and tissue resilience, could ensure personalized management strategies. The development of advanced tracheostomy tube designs, incorporating pressure-limiting features, and their clinical evaluation could reduce the risk of cuff over-inflation and its associated complications.
Acknowledgements
The authors have nothing to acknowledge. This project received no external funding.
Conflict of interest statement
None declared.
Funding
None declared.



