-
PDF
- Split View
-
Views
-
Cite
Cite
Suleiman Khaddour, Ahed Assaf, Saja Karaja, Mousa Barboura, William Borghol, Khaled Isa, Mesh migration to the sigmoid colon complicated by the formation of colocutaneous fistula 36 years post incisional hernia repair: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 5, May 2025, rjaf306, https://doi.org/10.1093/jscr/rjaf306
Close - Share Icon Share
Abstract
This article provides clinical insights into a rare instance of mesh patch migration complicated by colocutaneous fistula formation occurring post incisional hernia repair operation in a 67-year-old male. Our patient had a history of laparotomy due to a gunshot wound, followed by the development of an incisional hernia which was subsequently repaired with mesh implantation. Further examinations suggested mesh migration to the sigmoid colon, necessitating him to undergo laparotomy. While some complications from mesh placement are well known, mesh migration to the sigmoid colon remains an extremely rare complication, particularly after such an extended period, and only reported in the literature in few cases with inguinal hernia. This case underscores the importance of considering mesh migration, although rare, as a potential diagnosis in patients with prior hernia repairs, regardless of the elapsed duration since surgery. It emphasizes the need for further research to establish follow-up guidelines for patients with mesh placement (refer to graphical abstract).
Introduction
Mesh is used in incisional hernia repairs that occur at the site of a previous surgical intervention on the abdominal wall, with the aim of reducing the rate of hernia recurrence. Mesh types vary depending on the patient’s condition. The most commonly used mesh is the ‘permanent synthetic’ mesh, while the ‘absorbable’ mesh may be used in cases of infection [1]. Regardless of the type of mesh used, its use in hernia repair carries the risk of several complications, as occurs with any abdominal surgery, such as adhesions. Specific complications may also occur, such as mesh infection, fistula formation, mesh migration, and even recurrence of the previous hernia [2, 3]. In many cases, mesh migration into the abdominal cavity is associated with subsequent complications such as infection and fistula formation, as well as intestinal obstruction due to severe adhesions. Incomplete peritoneal repair may also contribute to mesh migration into the gastrointestinal tract, as the normal peritoneum normally separates the graft from the abdominal organs [3]. In this case report, we discuss a case of mesh migration accompanied by colocutaneous fistula which developed 36 years after repair of an incisional hernia resulting from a previous laparotomy for the gunshot wound management. Note that mesh migration into the colon is considered an extremely rare complication, especially with incisional hernias [4].
Case report
A 67-year-old male, with a smoking history of 40 pack-years, presented to the emergency department with an enterocutanous fistula. His medical history includes a prior laparotomy due to a gunshot wound, followed 6 months later by the development of an incisional hernia requiring surgical repair with the placement of a mesh patch. After 36 years of hernia repair operation, he developed an abscess, which was subsequently diagnosed and drained in another hospital. Three months post abscess drainage, the patient developed an enterocutanous fistula. On clinical examination, he exhibited grade II exertional dyspnea, orthopnea, and nocturnal paroxysmal dyspnea, with diminished breath sounds but no chest pain. Laboratory tests revealed normal urea and creatinine levels, mild anemia with a hemoglobin level of 10.8 g/dl, and elevated C-reactive protein at 150.4 mg/dl. Echocardiography and electrocardiography were both normal. A superficial abdominal ultrasound (US) detected a hyperechoic lesion with posterior acoustic shadowing extending 2 cm at the fistula opening, preventing clear visualization of any abdominal cavity connection. Moderate grade II edema was noted around the fistula opening in the subcutaneous tissue, without clear abscess formation (Fig. 1). A computed tomography (CT) scan was performed; the abdominopelvic CT scan findings indicate post-surgical changes in the abdominal region, including edema and air collections at the surgical site, without an assessment of an enterocutanous fistula. Chest CT findings were unremarkable, with no evidence of mediastinal lymphadenopathy. The heart and great vessels were of normal size (Fig. 2). Following a cardiology consultation confirming that surgical intervention was safe based on the patient’s normal laboratory parameters, an exploratory laparotomy was performed via a midline incision extending both above and below the umbilicus. The incision was carefully deepened through the abdominal wall into the peritoneal cavity. Initial exploration revealed a colocutaneous fistula; tracing the fistulous tract demonstrated that it terminated at the sigmoid colon. Further inspection uncovered a migrated surgical mesh that was wrapped and strongly adherent to the sigmoid colon. With considerable difficulty and utmost care, the displaced mesh was excised along with the resection of ~4 cm of the sigmoid colon. An end-to-end anastomosis of the sigmoid colon was then performed. Additionally, two tubular surgical drains were placed—one in the Douglas pouch and another at the splenic flexure of the colon—to facilitate post-operative drainage. Hemostasis was achieved with thorough drying, followed by layered closure of the wound after proper disinfection, and the application of a sterile dressing (Fig. 3). Following surgery, the patient was prescribed a regimen including antibiotics— ceftriaxone at 1 g twice daily and metronidazole at 500 mg three times daily—to manage infection risk. Intravenous paracetamol was administered every 8 hours for pain control. The patient was discharged in stable condition two days after surgery and a follow-up period of 6 months indicated no further complications.
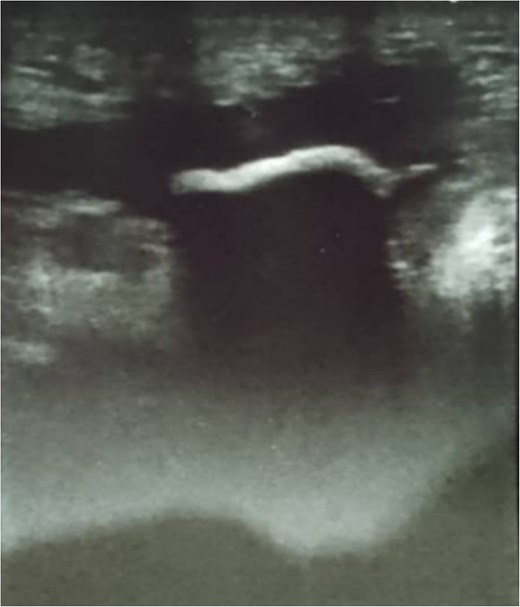
Superficial abdominal ultrasound showing a hyperechoic lesion with posterior acoustic shadowing extending 2 cm at the fistula opening, limiting visualization of any abdominal cavity connection. Moderate grade II edema is seen in the surrounding subcutaneous tissue, with no clear abscess formation.
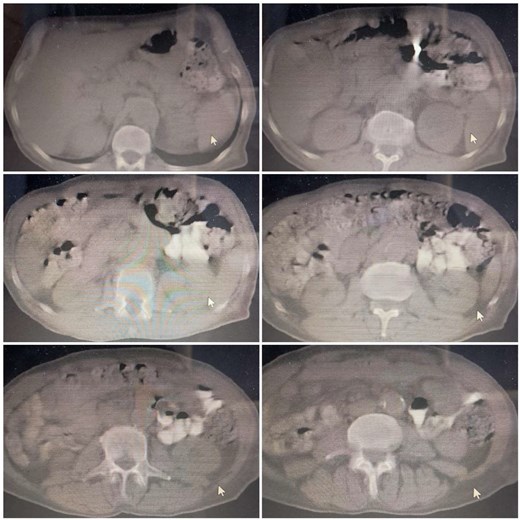
Abdominopelvic CT scan showing post-surgical changes in the abdomen without clear evidence of colocutaneous fistula. The chest findings are unremarkable.

Intraoperative findings during exploratory laparotomy revealing a displaced mesh strongly adhered to the lumen of the sigmoid colon. The surgical procedure involved removal of the mesh, resection of 4 cm of the sigmoid colon, and an end-to-end anastomosis.
Discussion
Incisional hernias can develop months or even years following abdominal surgery on the incision site. While most post-surgical incisions fully recover restoring a strong abdominal wall, impaired healing may decrease its strength resulting in organs or tissues expanding from the surgical scar [5]. Our patient had a history of prior laparotomy due to a gunshot wound followed by the development of an incisional hernia. Incisional hernias repair operation involves suturing the orifice and commonly supporting it with a synthetic mesh. Solicitous care to right placement, reliable suturing and following disinfectant protocols during hernia repair surgery are fundamental to avert complications related to the mesh [4–6]. Various complications are associated with mesh patch implantation, including visceral adhesions and abscesses. However, mesh migration is a rare and serious complication [4]. Several factors seem to influence the occurrence of mesh complications, including the type of hernia as complications are more likely with large, recurrent or parastomal hernias, type of mesh as polypropylene mesh has favoured advantages in hernia repair operations compared to other mesh types, the implantation technique as laparoscopic methods reduce complications rate compared to conventional techniques, and factors related to the patient as infections and delayed healing increase the complications rate [2, 4]. The occurrence rates of mesh migration, erosion or the perforation of nearby organs are not certainly known, as most existing data stem from individual reported cases. The clinical symptoms may differ widely based on the varying position of the migrating mesh, as most documented cases of mesh migration reported lower abdominal pain accompanied by mild tenderness [6]. Typically, mesh migration potentially emerges anywhere from 1 to 20 years following hernia repair operation though in most instances of mesh migration, the urinary bladder or intestines were involved. However, mesh migration to the sigmoid colon is extremely rare, and is reported in the literature as a complication of inguinal hernia repair [4, 6]. Remarkably, our patient developed the complications of mesh migration 36 years post hernia repair. The causes of mesh migration are classified into two categories: primary and secondary. Primary migration is related to the initial operation, as typically during the hernia repair operation, the mesh patch is attached to the abdominal wall using non-absorbable tackers, followed by the reconstruction of the peritoneum with interrupted trackers to encase the mesh. If either of these tackers is not secure, the poorly secured mesh shifts towards the least resistance planes, and may erode into the adjacent viscera [2, 6]. While secondary migration occurs due to infection, inflammation or reaction to foreign object [2, 6]. When migration occurs into the bowel, it may result in further complications such as obstruction and infection. However, fistula formation represents a rare complication, and multimodal imaging utilizing CT and US plays a crucial role in assessing mesh migration by providing insights on the extent of involvement and the suitable treatment [2]. Collapsed mesh is often identified on US as echogenic structure in an unusual location. If radiodense tackers are utilized, it may assist in detecting the mesh on CT scans [2]. As a treatment, it is recommended to fully remove the migrated mesh through laparotomy or laparoscopy, together with the partial or complete resection of the affected organ [6].
Conclusion
This case highlights the need for further research to provide follow-up guidelines for patients with mesh implantation. Surgeons must always ensure a proper secure suturing of mesh patches to prevent further complications. Although mesh migration and its complications are rare, clinicians should consider it as a differential diagnosis in patients with a history of hernia repair utilizing mesh patches irrespective of the elapsed duration following hernia repair operation. The long elapsed duration exceeding 20 years following hernia repair should not exclude the possibility of mesh migration.
Acknowledgements
Assistance with the study: the authors would like to express their sincere gratitude to:
Dr. Suleiman Amin, Head of General Surgery Department, Douma Hospital, Damascus, Syria; for supervising the surgical procedure.
Dr. Mahmoud Krenbeh and Dr. Alaa Deeb, Department of General Surgery, Douma Hospital, Damascus, Syria; for their assistance with data curation.
Conflict of interest statement
The authors declare no conflicts of interests.
Funding
No funding was provided for this study.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.



