-
PDF
- Split View
-
Views
-
Cite
Cite
Abdellatif Khader, Khaled Abbadi, Ammar Khader, Asil Musleh, Malvina Asbah, Oadi N Shrateh, Incidentally discovered large ancient retroperitoneal schwannoma: a rare case report and literature review, Journal of Surgical Case Reports, Volume 2025, Issue 5, May 2025, rjaf303, https://doi.org/10.1093/jscr/rjaf303
Close - Share Icon Share
Abstract
Ancient schwannoma is a rare retroperitoneal tumor that often remains asymptomatic and is frequently misdiagnosed. We present a case of a 16-year-old male with acute appendicitis, where a contrast-enhanced computed tomography scan incidentally revealed a well-defined cystic retroperitoneal lesion. The patient underwent appendectomy and enucleation of the mass. Histopathological analysis confirmed ancient schwannoma, showing Antoni A and B areas, degenerative changes, and positive S100 staining. Postoperative recovery was uneventful, with no recurrence at 6 months. This case underscores the importance of thorough imaging evaluations, even when assessing unrelated conditions, as incidental findings like ancient schwannoma can significantly impact patient management. Early diagnosis and complete surgical excision offer favorable outcomes.
Introduction
Retroperitoneal tumors encompass a diverse range of sarcomas and other benign or malignant lesions, with sarcomas being the most frequent type, accounting for ~1%–15% of all neoplasms in adults and children. Benign retroperitoneal tumors, however, are significantly less common than sarcomas, comprising ~40% of retroperitoneal tumors and often discovered incidentally. Among the most prevalent benign tumors in the retroperitoneal region are neurogenic tumors such as schwannomas and neurofibromas, as well as fibromatosis and renal angiomyolipomas [1].
Schwannoma is a tumor of soft tissue originating from Schwann cells of the peripheral nerve sheath. Therefore, it can appear in any Schwann cell of the nervous system, including trunks and extremities, but rarely occurs in the retroperitoneum region (only 0.5%–5% of all schwannomas) [2]. We present the case of a 16-year-old male initially diagnosed with acute appendicitis, who was subsequently found to have an incidental retroperitoneal ancient schwannoma. The case report is consistent with the SCARE 2023 guideline [3].
Case presentation
A 16-year-old male with no significant past medical or surgical history presented to the Accident and Emergency Department with a chief complaint of progressively worsening abdominal pain. The pain began 12 hours prior to presentation, initially localized to the periumbilical region before migrating to the right lower quadrant. The patient described the pain as sharp and constant, accompanied by nausea, loss of appetite, and low-grade fever. He denied any urinary symptoms, changes in bowel habits, or recent trauma.
On examination, he appeared mildly distressed with tenderness and guarding in the right lower quadrant. A positive McBurney’s point tenderness and rebound tenderness were noted. Laboratory investigations revealed mild leukocytosis with a left shift, suggestive of an inflammatory process.
Given the clinical suspicion of acute appendicitis, a contrast-enhanced computed tomography (CT) scan of the abdomen and pelvis was performed (Fig. 1). The imaging confirmed acute appendicitis, demonstrating a fluid-filled and dilated appendix measuring up to 1 cm with periappendiceal fat stranding and free fluid. Additionally, an incidental finding of a well-defined, thin-walled, unilocular cystic lesion in the retroperitoneum, located inferior to the aortic bifurcation and anterior to the L5 vertebral body, was observed. The lesion measured ~6 × 6 × 6.5 cm and showed mild enhancement, raising the differential of a mesenteric cyst or neurogenic tumor.

The images provided show axial and sagittal CT views of a well-defined retroperitoneal mass located anterior to the L5 vertebra. The lesion appears encapsulated, homogenous, and slightly hypodense compared to surrounding structures.
The patient was taken to the operating room for an appendectomy, during which the retroperitoneal mass was identified and excised (Fig. 2). The excised mass was encapsulated, soft, and hemorrhagic on cut section. Both specimens were sent for histopathological analysis.
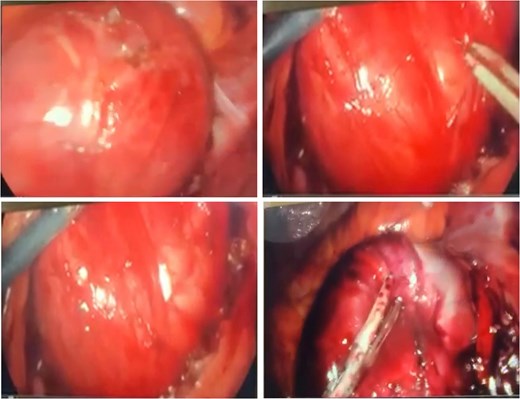
The intraoperative images depict the surgical excision of a large, encapsulated retroperitoneal mass. The mass appears smooth, well-circumscribed, and vascularized, consistent with the gross appearance of a benign tumor. Surgical instruments are shown mobilizing the mass, carefully dissecting it from surrounding tissues without significant invasion into adjacent structures.
Histopathological examination revealed a well-circumscribed encapsulated tumor with a biphasic pattern, comprising hypercellular Antoni A areas and hypocellular Antoni B areas. Nuclear palisading and Verocay bodies were identified, along with degenerative nuclear atypia and cystic changes consistent with the diagnosis of an ancient schwannoma. No evidence of malignancy was found (Fig. 3).
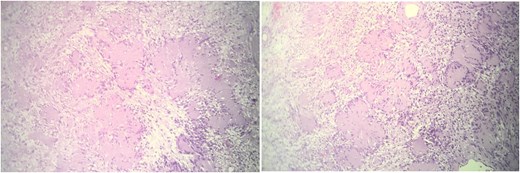
These histological images demonstrate a well-circumscribed tumor with distinct biphasic architecture, characteristic of schwannomas. The hypercellular Antoni A areas, marked by closely packed spindle cells arranged in a palisading pattern, are interspersed with hypocellular Antoni B regions, which exhibit loosely arranged spindle cells within a myxoid stroma. Additionally, degenerative changes, including cystic spaces and evidence of hyalinization, are evident, aligning with the features of an ancient schwannoma. The absence of mitotic figures or necrosis suggests the benign nature of the lesion. This histological presentation, combined with clinical and imaging findings, confirms the diagnosis of an ancient schwannoma.
The patient had an uneventful postoperative course and was discharged on the third postoperative day. At follow-up, he remained asymptomatic with no signs of recurrence or complications. Further imaging and clinical evaluations are planned to monitor for potential recurrence, given the rare nature of retroperitoneal schwannomas.
Discussion
Retroperitoneal schwannoma is a solid, encapsulated benign tumor that typically originates in the paravertebral region. On gross examination, it presents as a solitary, well-defined mass with a smooth surface. Histologically, schwannoma is composed of Schwann cells displaying alternating hypercellular (Antoni A) and hypocellular (Antoni B) areas, and it demonstrates positive staining for S100 protein. The presence of degenerative features, such as cystic changes, hemorrhage, calcification, and hyalinization, characterizes a specific subtype known as ancient retroperitoneal schwannoma [2].
Due to the flexibility of the retroperitoneal space, retroperitoneal schwannomas can grow slowly to a significant size without invading adjacent structures. As a result, these tumors often remain clinically silent in their early stages and are typically not detected until they exert pressure on surrounding organs [2]. Common symptoms of retroperitoneal schwannomas include abdominal pain and nonspecific gastrointestinal disturbances, such as discomfort during defecation, as well as other symptoms like hematuria and recurrent renal colic [4]. In the present case, the ancient schwannoma was discovered incidentally during the investigation of an unrelated condition—acute appendicitis.
Imaging techniques commonly used to detect retroperitoneal schwannomas include abdominal ultrasound, CT scans, and magnetic resonance imaging (MRI) [2]. Ultrasound typically reveals a homogenous, well-defined, and poorly vascularized lesion, although some studies have described central cystic areas with necrotic heterogeneity. CT scans often show a cystic mass with central necrosis, characteristic of schwannomas [5, 6]. In this case, the patient underwent a CT scan, which revealed findings consistent with acute appendicitis, including a fluid-filled and dilated appendix measuring up to 1 cm with surrounding periappendiceal fat stranding and minimal free fluid. Additionally, the CT scan incidentally identified a thin-walled, slightly enhancing unilocular cystic lesion in the retroperitoneum, located inferior to the aortic bifurcation and anterior to the L5 vertebral body. The lesion measured ~6 × 6 × 6.5 cm and displayed features suggestive of a benign retroperitoneal tumor, such as a well-defined and encapsulated appearance. These imaging findings, combined with surgical excision and histopathological analysis, confirmed the diagnosis of an ancient schwannoma. While procedures such as biopsy or CT-guided fine-needle aspiration biopsy can help confirm the diagnosis, they are generally avoided preoperatively due to the risk of complications like bleeding, infection, or tumor seeding [2].
Complete surgical excision, including adjacent tissue, if necessary, is considered the optimal treatment for retroperitoneal schwannoma [2, 4–6]. However, some studies suggest that simple enucleation or partial excision may be sufficient due to the low risk of malignant transformation associated with retroperitoneal schwannomas [2, 6]. In this case, we opted for simple enucleation of the tumor without removing adjacent tissue, as the imaging findings were consistent with a benign retroperitoneal lesion, demonstrating no invasive characteristics or signs suggestive of malignancy.
Retroperitoneal schwannomas typically have a favorable prognosis, with recurrence reported in 5%–10% of cases, often attributed to incomplete excision [4]. Postoperative imaging, such as CT or MRI, is generally recommended within 6–12 months to monitor for recurrence [4–6]. In this case, we achieved complete excision of the tumor during surgery. At the 6-month follow-up, no evidence of recurrence was observed. However, further studies are required to validate and optimize our management approach and follow-up protocols.
Conclusion
Ancient schwannoma is a rare subtype of retroperitoneal schwannoma that often remains clinically silent or is misdiagnosed as other conditions. The diagnosis can be reliably established through imaging studies, followed by postoperative histopathological examination. While imaging aids in identifying characteristic features such as cystic degeneration and encapsulation, histopathology confirms the diagnosis through findings like Antoni A and B patterns, S100 protein positivity, and degenerative changes. However, there is ongoing debate regarding the requirement for achieving negative tissue margins during surgery, as some evidence suggests that enucleation or partial excision may suffice given the low likelihood of malignant transformation.
Author contributions
O.N.S., M.A., A.M., and K.A. contributed to writing the manuscript. M.A., A.M., K.A., and O.N.S. contributed to imaging description. A.K. and A.K. contributed to reviewing & editing the manuscript.
Conflict of interest statement
None declared.
Funding
No funding or grant support was received for this study.
Ethical approval
Our institution has exempted this study from ethical review.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Guarantor
Oadi N. Shrateh



