-
PDF
- Split View
-
Views
-
Cite
Cite
Takahiko Sakuma, Hidemichi Yuasa, Melanocytic nevus of the gingiva associated with mirror-image bi-nucleated cells, nuclear inclusion bodies, and apoptotic bodies: a case report and review of the literature, Journal of Surgical Case Reports, Volume 2025, Issue 4, April 2025, rjaf221, https://doi.org/10.1093/jscr/rjaf221
Close - Share Icon Share
Abstract
A case of melanocytic nevus of the gingival mucosa is reported. In a 16-year-old female, tiny black papules were clustered in an area of approximately 2 mm in diameter on the maxillary gingiva. Each papule was clearly demarcated from the surrounding healthy gingival mucosa. A resection biopsy revealed a melanocytic nevus. Each nevus cell nest was clearly separated from neighbouring nests and appeared benign on low power view. However, at high power, pigmented cells associated with mirror-image two-nuclei, nuclear inclusion bodies, and apoptosis were occasionally observed. Pigmented cells were diffusely stained with S100 protein but not HMB45. The Ki-67 (MIB-1) labelling index was very low. The lesion was diagnosed as a benign melanocytic nevus of the gingiva. In contrast to cutaneous melanocytic nevi, pigmented lesions of the gingiva, including the oral cavity, are rare. The pathological findings are described in detail and discussed with a review of the literature.
Introduction
Melanocytic lesions in the oral cavity are rare. A small number of cases have been reported sporadically, mostly as single-case reports. Dentists, oral surgeons, and pathologists are not familiar with pigmented lesions and may have difficulties in clinical management and pathological diagnosis. We present a case of gingival melanocytic nevus. The macroscopic and microscopic findings and their relationship to clinical significance are discussed with a brief review of the literature.
Case report
In a 16-year-old female, a cluster of small black papules on the right maxillary gingiva (buccal side) was found by a local general dentist during routine dental care. The patient was unaware of the lesion as it was completely asymptomatic. The patient was referred to our hospital one week later and inspection of the entire oral cavity revealed no other abnormalities. She had no past history of dentures treated with amalgam prosthetics. The lesion was clearly demarcated from the surrounding healthy gingiva (Fig. 1), and there was no ulceration or induration around the lesion.

Macroscopic view of the lesion. A cluster of tiny black papules was observed in the gingiva just above the right canine tooth.
For pathological examination of the lesion, incision biopsy was performed. Under local anaesthesia with an injection of 1 ml 2% lidocaine hydrochloride (containing 1:80 000 adrenaline), the lesion was excised with a margin of 1 mm. This also resulted in complete removal of the lesion. The periosteum of the underlying maxillary bone was grossly intact. The gingival mucosa was sutured and, with the prescription of oral analgesics and antibiotics, the wound healed within one week.
The lesion was composed of multiple nests of nevus cells, each nest corresponding to a small black papule under low-power magnification (Fig. 2A). This lesion looked like a melanocytic nevus, as often seen in the skin, in which the nevus cells closer to the stratified squamous epithelium had cytoplasmic melanin pigment (Fig. 2B). Microscopically, at low power, the nevus cell clusters were well demarcated from the surrounding stroma, and the lesion appeared benign as a melanocytic nevus commonly seen in the skin. However, haematoxylin-eosin (HE) staining at high power revealed anisonucleosis, irregular nuclear shape, and enlarged nucleoli. Most importantly, bi-nucleated cells, often as mirror-image (Fig. 2C), and apoptotic bodies (Fig. 2D) were occasionally seen. Many nuclear inclusion bodies were also observed (Fig. 2C and D). However, mitotic figures were absent. Immunohistochemically, the nevus cells were diffusely stained with S-100 (Fig. 2E) but negative for HMB-45 (not shown). Ki-67 immunohistochemistry stained only stem cells in the basal layer of the stratified squamous epithelium, leaving the nevus cells unstained (Fig. 2F). Although the nuclear findings on HE staining raised concerns about the neoplastic nature of the lesion, the lesion was diagnosed as a benign melanocytic nevus of the gingiva. After resection, the clinical course has been uneventful.
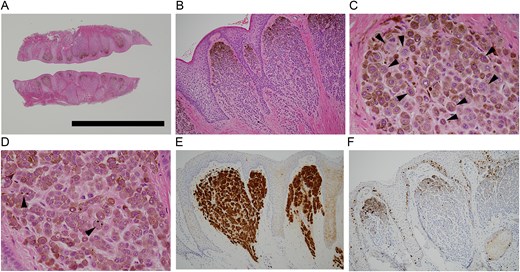
(A) Whole-mount view of the gingival lesion. The incision biopsy sample was halved along the longitudinal axis and mounted vis-à-vis. Note that the lesion is slightly raised symmetrically, and foci of nevus cell clusters are present beneath the surface epithelium. (Solid bar = 3 mm). (B) Histology of the biopsied lesion. In each focus of nevus cell clusters, the nevus cells near oral cavity were endowed with melanin pigment (HE, ×100). (C) In the pigmented cell clusters, multiple mirror-image bi-nucleated cells were noted (arrowheads). Nuclear inclusion bodies were also seen (HE, ×400). (D) In the pigmented cell foci, apoptosis bodies were observed (arrowheads). Nuclear inclusion bodies were also seen in this field (HE, ×400). (E) Pigmented cells were uniformly stained with S-100 (×100). (F) Pigmented cells were scarcely stained with Ki-67. Only basal layer cells of stratified squamous cell epithelium were labelled (×100).
Discussion
A case of melanocytic nevus of the gingiva in an adolescent female is described. This case was remarkable in that the macroscopic features did not agree well with the microscopic findings. Grossly, small black papules were well-defined and clearly demarcated. Macroscopically, no pigment permeation into the surrounding healthy gingival mucosa was observed (Fig. 1). Histologically, anisonucleosis, irregular nuclear shape, prominent nucleoli, bi-nucleated cells often as mirror images (Fig. 2C), and apoptotic bodies (Fig. 2D) were noted on high-power HE staining, although mitotic figures were absent on HE staining. We were puzzled as to how to interpret these seemingly contradictory findings to arrive at a pathological diagnosis. HMB-45 was negative (not shown), and Ki-67-labelled cells in the specimen were restricted to the basal layer of the stratified squamous epithelium, sparing the nevus cells in the foci (Fig. 2F). Immunohistochemistry allowed us to conclude that this lesion was a benign melanocytic nevus of the gingiva.
While melanocytic nevi of the skin is a very common dermatological disease, melanocytic lesions occurring in the oral cavity are rare. In a classic case series of intra-oral melanocytic lesions [1], pigmented nevi accounted for only 0.15% of oral surgical specimens. Excluding racial and exogenous pigmentation such as amalgam tattoos, heavy metals, smoking, and drug-induced pigmentation, oral melanocytic lesions include nevi, melanoma, melanoacanthoma, and melanotic neuroectodermal tumour of infancy [2]. As with cutaneous melanocytic nevi, there are several subtypes of oral mucosal melanocytic nevi. Of these, the intramucosal type is the most common [1–3], followed by the compound nevus [3] or blue nevus [1, 2]. The order of the second and subsequent subtypes differed among reports. However, the junctional type is the least common type of oral melanocytic nevus [1, 2]. In one study, junctional nevi showed an increased risk of melanoma among the subtypes of melanocytic nevi [4].
The site where melanocytic lesions arise most frequently in the oral cavity is hard palate [1, 2]. Other locations include buccal membrane, gingiva, lip, etc.; the order of incidence varies according to the reports.
The age distribution of oral nevi also differs from report to report: the most common age interval is the twenties [3, 5], thirties [3, 5], or forties [2]. However, teenagers, as in our case, are less frequently affected, varying from 2.2% [2] to 19% [5].
In contrast to their dermal counterparts, dentists and pathologists have little experience and knowledge of melanocytic lesions in the oral cavity. Melanocytic lesions in the oral cavity are poorly understood compared to those in the skin. Therefore, caution should be exercised in the diagnosis of oral melanocytic lesions. Macroscopic observation alone, which is common in dermatology clinical practice, is not reliable for assessing the potential malignant risk of oral melanocytic lesions. It is recommended that all melanocytic-pigmented lesions in the oral cavity be resected and submitted for histological examination [3].
We believe that the macroscopic and microscopic images presented here are informative for both dentists/oral surgeons and pathologists and may be useful in the diagnosis and management of patients. If there is a conflict of findings regarding the diagnosis, other ancillary diagnostic tools, such as immunohistochemistry should be used without hesitation.
This report describes detailed histological findings of gingival melanocytic nevi, which are poorly understood due to the rarity of the cases. This would be useful information for readers. However, this is a single case report, so the information obtained here is limited, and therefore our interpretation should be further investigated in future studies.
Conflict of interest statement
None declared.
Funding
None declared.



