-
PDF
- Split View
-
Views
-
Cite
Cite
Peter Tilleard, Nathan Brunott, Caecal obstruction secondary to a Meckel’s diverticulum, Journal of Surgical Case Reports, Volume 2025, Issue 4, April 2025, rjaf210, https://doi.org/10.1093/jscr/rjaf210
Close - Share Icon Share
Abstract
A Meckel’s diverticulum is the most common congenital anomaly of the gastrointestinal tract, with a population incidence of approximately 2%. They are known to cause several complications including obstruction, haemorrhage, tumours, infection, and perforation. The vast majority however are asymptomatic and therefore provide a management conundrum when discovered incidentally. We report the case of a 71-year-old female who presented with abdominal pain and bloating. She was taken for a diagnostic laparoscopy which revealed a partial caecal obstruction secondary to a fibrous band running from a Meckel’s diverticulum around the caecal pole to the mesentery. The band had likely been severed from the umbilicus but not resected at a previous surgery. The caecal obstruction was relieved and the diverticulum resected uneventfully. This rare case underscores the variety of complications that a Meckel’s diverticulum can cause and highlights the difficult management decision when faced with an asymptomatic incidentally found Meckel’s diverticulum.
Introduction
The vitelline duct (omphaloenteric duct) in a foetus serves to connect the yolk sac to the intestinal tract [1]. Incomplete obliteration of this duct can result in a variety of abnormalities, the most common of which is a Meckel’s diverticulum (MD) [1]. A MD is a true diverticulum of the small bowel, it has a reported prevalence of between 0.3% and 2.9% and is found on the antimesenteric surface of the mid to distal ileum [1, 2].
Intestinal obstruction is a common complication associated with a MD. Other complications include haemorrhage, tumours, infection, and perforation. Obstruction can be caused by the MD acting as a lead point and causing intussusception of the small bowel. This process is more common in the paediatric population [2]. Other mechanisms by which a MD may cause a bowel obstruction are related to the attached bands which may be present [1, 3, 4]. A MD may or may not have associated fibrous bands running to the mesentery (mesodiverticular band) or the umbilicus [1, 4].
A band running from a MD to the umbilicus is a continuation of the incompletely obliterated vitelline duct [4]. A mesodiverticular band is the incompletely obliterated remnant of the foetal vitelline artery, it runs from the tip of the MD to the mesentery of the ileum creating a snare like opening [5]. Both types of bands are known to cause small bowel obstruction however there are only limited reports of caecal obstruction [4–7].
Of those patients with a MD the vast majority are thought to be asymptomatic, with the lifetime risk of developing a complication reported between 4.2% and 6.4% [8, 9]. There is a variety of practice in surgeons’ approaches to the incidentally found asymptomatic MD. A study of 1476 patients at the Mayo Clinic failed to support or reject the approach of resecting all incidentally found asymptomatic diverticula [10]. The study did however suggest that any MD with one of their four high risk criteria (age less than 50 years, male sex, diverticulum length greater than 2 cm, presence of histologically abnormal tissue) should be prophylactically resected [10].
Resection of a MD can be achieved by either simple diverticulectomy or segmental resection and primary anastomosis. An Australian study showed that while a long (length twice the diameter) MD can be safely removed by simple diverticulectomy, a short MD should be removed by segmental resection because of the uncertainty of the site of potential ectopic mucosa within the MD [11]. In addition, consideration should be given to segmental resection if there is a palpable abnormality at the base of the diverticulum or if it is thought simple diverticulectomy might result in narrowing of the intestinal lumen.
Case report
We report the case of a 71-year-old female who presented with a long history of abdominal pain and cramps since childhood. These symptoms had increased and been associated with bloating since a recent bout of uncomplicated sigmoid diverticulitis which was managed conservatively. She had recently had a colonoscopy which had failed to identify any abnormality. A computed tomography (CT) scan showed a distended caecum and suggested a degree of stenosis in the proximal ascending colon (Fig. 1). Her surgical history included an upper midline laparotomy extending to the umbilicus for an open cholecystectomy and an abdominoplasty.
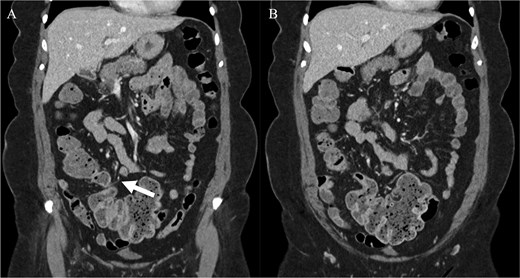
Computed tomography imaging of the patient pre-operatively. (A) The structure suspected to be the band partially obstructing the caecum is indicated by the arrow. (B) The distension of the caecum prior to the obstructing band is demonstrated.
She underwent a diagnostic laparoscopy which identified a partial caecal obstruction secondary to a fibrous band running from a Meckel’s diverticulum around the caecal pole to the small bowel mesentery (Fig. 2). It did not have the typical appearance of a mesodiverticular band and was thought to have been a band running from the MD to the umbilicus which had been let down from the umbilicus at her previous laparotomy and subsequently implanted itself in the small bowel mesentery. The band was untwisted from around the caecum. Simple diverticulectomy of the MD and its band was performed. The patient recovered uneventfully. She was subsequently seen in the out-patient clinic and reported resolution of her symptoms.
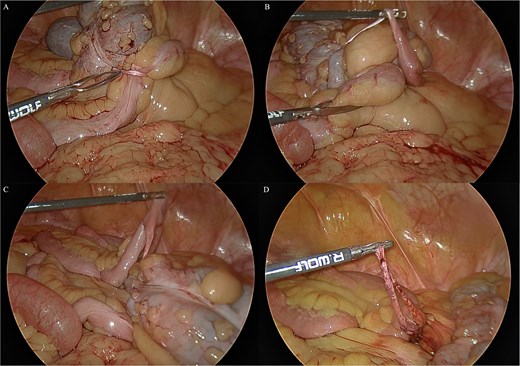
Intraoperative laparoscopic views. (A) The band is seen wrapped around the caecum causing the partial obstruction. (B) The band is untwisted from around the caecum and the Meckel’s diverticulum is revealed. (C) The Meckel’s diverticulum and its band are examined. (D) The band is transected.
Discussion
Approximately 2% of the population have a MD, of these only a small percentage will ever become symptomatic. A symptomatic MD may mimic many other abdominal pathologies and is difficult to diagnose.
A MD with a fibrous band running to the umbilicus is a further rare subset of this congenital anomaly. This case highlights the importance of considering resecting these diverticulum when found incidentally. Previous authors discussing complications of diverticular bands have suggested that resection of either the diverticulum or at least the band is appropriate if found incidentally as they are possible sites of future obstruction [4–6]. This case supports this opinion.
This case demonstrates a rare sequela of an unresected MD and a safe workup and laparoscopic approach to this pathology.
Conflict of interest statement
None declared.
Funding
None declared.



