-
PDF
- Split View
-
Views
-
Cite
Cite
Bernarda Patiño-Araujo, María E Salgado-Báez, Gabriel P Villavicencio-Logroño, María J Ayora-Pérez, Gabriela S Zapata-Jaramillo, Napoleón Salgado-Macías, Early small bowel obstruction by phytobezoar related to zopiclone induced amnesia after revisional Roux-en-Y gastric bypass: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 4, April 2025, rjaf202, https://doi.org/10.1093/jscr/rjaf202
Close - Share Icon Share
Abstract
This case report details an unusual instance of small bowel obstruction occurring within 48 h after a successful Roux-en-Y gastric bypass (RYGB) procedure. A 59-year-old woman, who had undergone a revisional RYGB and was discharged 24 h post-surgery, returned to the emergency department with acute epigastric pain and vomiting at the 48-h mark. A contrast computed tomography scan revealed dilated small bowel loops, right pleural effusion, and some free gas. An emergency laparoscopy identified an obstruction at the jejunojejunal anastomosis caused by undigested food, including seeds. The obstructive material was removed, and the anastomosis was reconstructed. Subsequent psychiatric evaluation revealed the patient’s abuse of zopiclone, taken at four times the recommended dose. This misuse likely led to anterograde amnesia, resulting in unreported dietary indiscretions. This case underscores the importance of comprehensive medication history and patient education to mitigate risks associated with medication misuse and non-compliance.
Introduction
Bowel obstruction following Roux-en-Y gastric bypass (RYGB) is a recognized complication occurring in ⁓1.5%–11% of patients, with small bowel obstruction (SBO) accounting for 1.8% of these cases [1]. SBO can be categorized based on the time of onset: early, within 30 days post-surgery, or late. Early obstructions often stem from surgical technical errors or dietary noncompliance, whereas late obstructions may result from adhesions or other complications [2]. Only 1.2% of SBO occurs within 30 days after surgery [3]. Phytobezoars represent a rare cause of SBO, particularly following RYGB. They account for ˂1% of SBOs after this type of surgery [2]. They are the most common type of bezoar, and bariatric surgery increases their risk by allowing unhydrolyzed food particles to pass into the small intestine. Phytobezoars usually present as a rare late complication [4].
Zopiclone is a nonbenzodiazepine hypnotic used to manage insomnia, with a maximum recommended dosage of 7.5 mg daily. Although anterograde amnesia is a known but rare side effect of zopiclone, it is more likely to occur at higher doses [5]. Though no specific data was available for Zopiclone, sleep- related eating disorder has been reported in 6.2% of patients using Zolpidem, another z-drug [6, 7]. The patient in this case did not initially report zopiclone use. However, a subsequent psychiatric evaluation revealed frequent self-medication with this hypnotic, contributing to her postoperative complications.
This case report is notable for describing a phytobezoar-induced SBO occurring within 48 h of a technically sound surgical procedure. Since phytobezoar-related obstructions usually develop months or years after surgery, this case is particularly unusual.
Case report
A 59-year-old woman with a history of gastric sleeve surgery in 2019 presented with severe gastroesophageal reflux and weight regain, resulting in a body mass index of 31.41. Diagnostic evaluation included endoscopy, which revealed reflux esophagitis, a 3 cm hiatal hernia, a wide hiatus (Hill III-IV), gastric biliary reflux, and gastropathy in the gastric body and antrum. Histological analysis confirmed gastroesophageal reflux disease, and her glycosylated hemoglobin was 6.25%. Given these findings, a revisional laparoscopic RYGB with hiatoplasty was planned.
The laparoscopic RYGB was performed successfully. The surgical technique involved the creation of a gastrojejunostomy and jejunojejunostomy using a linear stapler. The patient was discharged 24 h post-surgery with comprehensive medical and nutritional instructions.
The patient returned to the emergency department 24 h after discharge, presenting with acute epigastric pain, vomiting, and headache. She reported no dietary indiscretions or issues with prescribed medications. Physical examination revealed abdominal distension and tenderness in the epigastric region, but there were no signs of peritonitis.
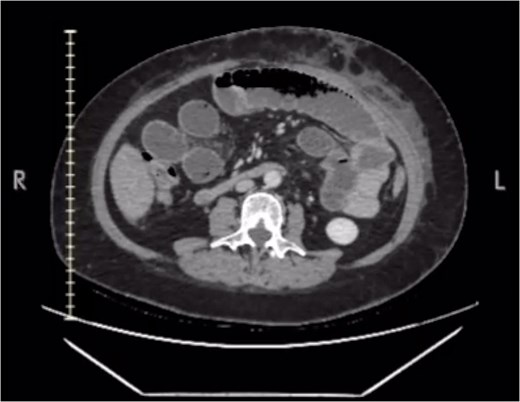
Laboratory tests indicated leukocytosis (13.4 × 103/μL) with neutrophilia (89.6%). A contrast-enhanced computed tomography (CT) scan demonstrated small bowel dilation up to the posterior distal suture (Fig. 1), mild right pleural effusion, and minimal free gas in the mediastinum. These findings suggested a small bowel obstruction, prompting an emergency diagnostic laparoscopy.
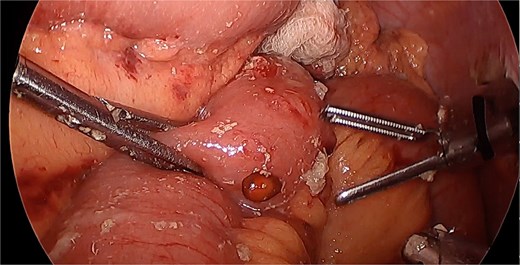
The laparoscopy revealed a preserved gastric pouch but distended small bowel loops. The anastomoses were intact. During the disassembly of the jejunojejunostomy, undigested solid food, including seeds, was found to be causing an intestinal obstruction (Fig. 2). This finding was consistent with a phytobezoar, which had led to the obstruction. The obstructing material was removed, and the anastomoses were reconstructed. Additionally, mesenteric gaps were closed, and a left subphrenic drain was placed to manage postoperative effusions and prevent further complications.
Postoperatively, the patient developed anuria and was diagnosed with abdominal sepsis and acute kidney injury (AKIN II). Adjustments to antibiotic and diuretic therapies were made, and parenteral nutrition was initiated to ensure adequate nutritional support during recovery. A psychiatric evaluation revealed that the patient had been self-medicating with zopiclone at four times the recommended dose (30 mg nightly), which was found to contribute to anterograde amnesia. This amnesia led to unrecognized dietary errors that contributed to the small bowel obstruction.
The management of the patient’s condition included psychiatric intervention to address the misuse of zopiclone. Quetiapine was prescribed to manage her sleep issues effectively, reducing the incidence of amnesic episodes and helping prevent further dietary indiscretions.
By the ninth postoperative day, the patient’s ileus resolved. Clear liquids were reintroduced, followed by liquid protein, as tolerated. The patient’s condition improved, sepsis was resolved, and she was discharged on the tenth day. Follow-up care included psychiatric, medical, and nutritional support to ensure ongoing recovery and to prevent future complications.
Discussion
This case highlights several critical aspects of postoperative care following bariatric surgery. First, it underscores the importance of a thorough and accurate medical history, including a full disclosure of all medications, whether prescription or over-the-counter, and any self-medication practices. It is known that medication misuse can lead to significant postoperative complications, including rare and severe ones such as phytobezoar-induced SBO, as demonstrated in this case.
A study done in the Andean region of Ecuador reported that 54.4% of subjects acquire drugs without proper prescriptions [8]. This demonstrates how widespread self-medication is in our country.
Zopiclone, although effective for managing insomnia, can cause side effects such as anterograde amnesia, especially when used inappropriately or in higher doses [8]. The patient’s self-medication with zopiclone at doses far exceeding the recommended amount was a critical factor in the development of her postoperative complications. This case illustrates the importance of educating patients about the risks of self-medication and ensuring that they adhere to prescribed doses and guidelines.
The occurrence of a phytobezoar within 48 h post-surgery is unusual and demonstrates the need for careful monitoring of dietary intake and gastrointestinal function in the early postoperative period. The resolution of the ileus and the patient’s subsequent recovery emphasize the importance of prompt diagnosis and intervention in managing such complications.
In Ecuador, 25.6% of medication acquired without prescription were recommended by a family member and 23% by a pharmacy clerk (not required to be a pharmacist) [8]. In this context people might not realize the relevance of the medication used and dosage and might not be able to relay information to their medical team. A strong doctor-patient relationship is essential to obtain a complete medical history.
In conclusion, this case report serves as a reminder of the need for comprehensive patient evaluations and careful management of postoperative care. The importance of screening for high-risk medication as a potential source of postsurgical compliance errors that hinder recovery can prevent serious complications and improve patient outcomes.
Conflict of interest statement
None declared.
Funding
None declared.
References
- small bowel obstruction
- computed tomography
- select the dosage, dosage form or route of administration
- pleural effusion
- diet
- epigastric pain
- amnesia
- amnesia, anterograde
- anastomosis, surgical
- emergency service, hospital
- food
- intestine, small
- laparoscopy
- patient education
- seeds
- surgical procedures, operative
- vomiting
- psychiatric evaluation
- phytobezoars
- gastric bypass, roux-en-y
- zopiclone



